Research![]() | Volume 8, Article 37, 21 May 2025
| Volume 8, Article 37, 21 May 2025
Cholera outbreak in Hanang District, Manyara, Tanzania, July 2024: An unmatched case-control study
Peter Richard Torokaa1,2,&, Agnes Njau1,2, Jasper Kimambo1,2, Loveness Urio2, Victor Muchunguzi3, Robert Makala4, Ally Hussein2
1Muhimbili University of Health and Allied Sciences, School of Public Health and Social Sciences, Dar es Salaam, Tanzania, 2Tanzania Field Epidemiology and Laboratory Training Program, Dar es Salaam, Tanzania, 3Mzumbe University, Morogoro, Tanzania, 4Regional Health Management Team, Manyara, Tanzania
&Corresponding author: Peter Richard Torokaa, Muhimbili University of Health and Allied Sciences, School of Public Health and Social Sciences, Dar es Salaam, Tanzania, Email: petertorokaa@gmail.com ORCID: https://orcid.org/0009-0003-3843-3434
Received: 05 Mar 2025, Accepted: 20 May 2025, Published: 21 May 2025
Domain: Field Epidemiology, Outbreak Investigation,
Keywords: Tanzania, Manyara, Cholera outbreak, Hanang
©Peter Richard Torokaa et al Journal of Interventional Epidemiology and Public Health (ISSN: 2664-2824). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Peter Richard Torokaa et al Cholera outbreak in Hanang District, Manyara, Tanzania, July 2024: An unmatched case-control study. Journal of Interventional Epidemiology and Public Health. 2025;8:37. https://doi.org/10.37432/jieph-d-25-00061
Abstract
Introduction: Cholera, a secretory diarrheal illness caused by Vibrio cholerae, is a significant public health threat in low-income countries, resulting in 1.3 to 4.0 million cases and 21,000 to 140,000 deaths annually. Persistent cholera outbreaks in the country necessitate investigation, Water Sanitation and Hygiene (WASH) improvements, and strengthened response interventions. This study aimed to describe the outbreak, determine its source and risk factors and institute control measures to guide effective prevention and containment strategies.
Methods: We conducted a descriptive analysis of the cholera cases recorded in the line list. Data collection for the case-control study was done using Kobo Toolbox. The QGIS 3.26.3 was used to map the hotspot area. Categorical variables were summarized using frequency distributions, and binary logistic regression was applied to assess factors associated with cholera disease transmission. The measure of association was the Odds Ratio (OR) with corresponding 95% Confidence Intervals (CI). Statistical significance was set at a p-value of <0.05.
Results: We found an Attack Rate (AR) of (86/17146, 0.5%), and the majority of cholera cases were below 25 years 19/45 (42.2) than control 9/45 (20%). More than half of the cases (44/86, 51.2%) were female. A total of 79/86 (91.9%) cases were farmers. A total of 85/86 (98.8%) were residing in the Gisambalang ward, and 42/86 (48.8%) were from Gandi hamlet. The Case Fatality rate (CFR) was 3 (3.5%). We found that individuals below the age of 25 years had 4.05 times the odds of getting cholera (AOR 4.05, 95%CI: 1.45-11.26). Individuals who ate food outside their homes had 4.43 times the odds of getting cholera (AOR 4.43, 95%CI: 1.55- 12.63).
Conclusion: Overall, the cholera outbreak in Hanang district, specifically in Gisambalang ward, affected farmers. Also, the case fatality rate was high, 3.5%. The age below 25 years and eating outside the home was significantly associated with cholera transmission. We emphasize community education, personal hygiene and sanitation interventions.
Introduction
Cholera, a secretory diarrheal illness caused by Vibrio cholerae, is a significant public health concern, particularly in low-income countries. It causes between 1.3 and 4.0 million cases annually, resulting in 21,000 to 140,000 deaths globally, disproportionately affecting regions with lower socioeconomic status [1]. Cholera remains a serious of public health concern in Africa, with over 178,000 confirmed cases across 16 countries in Eastern and Southern Africa during 2024. Tragically, these cholera outbreaks started on January 2024, led to nearly 2,900 deaths, with most of the victims being children [2]. The World Health Organization (WHO) reported a sharp rise in cholera cases within the African Region, with January 2024 recording a 30% increase compared to the same period in 2023. This underscores the ongoing difficulties in controlling the disease [2].
As of 2022, nearly 120 million people in Eastern and Southern Africa, including 60 million children, were relying on contaminated water for drinking. About 22% of the population in the region lacked any access to clean water [2]. By March 2023 several countries reported cholera outbreak in Africa with highest case fatality rate such as South Africa 16.7%, Malawi 3.1%, Nigeria 2.6%, Ethiopia 2.2%, Kenya 1.6% [3]. Tanzania among the East African countries reported the current cholera outbreak which began in September 2023, initially affecting the Kigoma and Mara regions. By early December 2023, the outbreak was contained, with 692 cases and 13 deaths reported, resulting in a Case Fatality rate (CFR) of 1.9%.
However, on 23 December, 2023 the outbreak resurged in Simiyu Region. Since then, cholera outbreaks have been reported across 22 regions, including Mara, Arusha, Kilimanjaro, Kigoma, Kagera, Singida, Simiyu, Shinyanga, Tabora, Ruvuma, Mwanza, Geita, Rukwa, Dodoma, Manyara, Morogoro, Katavi, Pwani, Mtwara, Tanga, Lindi and Dar es Salaam), resulting in a total of 1265 cases and 23 deaths (CFR 1.8%) as of 28 May 2024 [3].
In Manyara region, the cholera outbreak started on 8 July 2024 as reported by the district team. The Ministry of Health, in collaboration with other sectors and partners has implemented several interventions in the fight against cholera. The Ministry of Health deployed national rapid response teams to work with the regional and district teams. These teams consisted of experts from the cholera response technical pillars of Risk Communication and Community Engagement (RCCE), Water Sanitation and Hygiene (WASH), Disease Surveillance, Point of Entry, Case Management and Infection Prevention and Control (IPC). Also three Tanzania Field Epidemiology and Laboratory Training Program (TFELTP) residents contributed in the response efforts by educating clinicians on surveillance tools, risk communication and community engagement and performed a case control study. The FELTP is crucial for global health security and strengthening outbreak response capabilities in Tanzania. The persistent cholera outbreaks in 22 regions across Tanzania and high CFR of 1.8%, necessitated this outbreak investigation to identify sources, improve WASH and strengthen interventions and capacity building essential to the response teams. This study aimed to describe the outbreak, determine its source, identify the risk factors and institute control measures to guide effective prevention and containment.
Methods
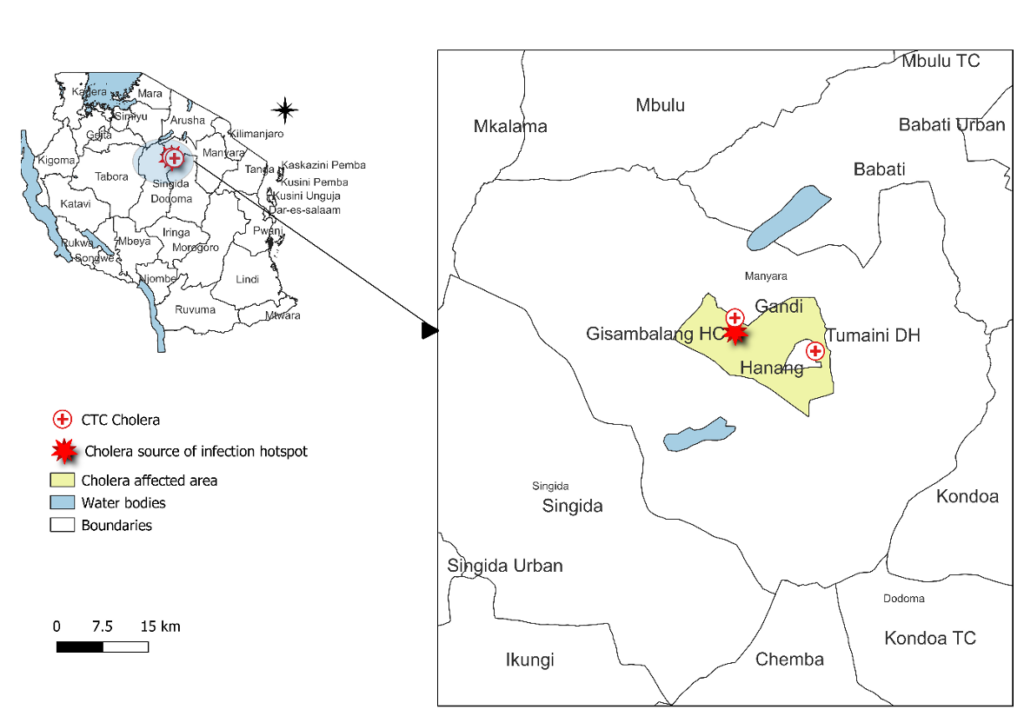
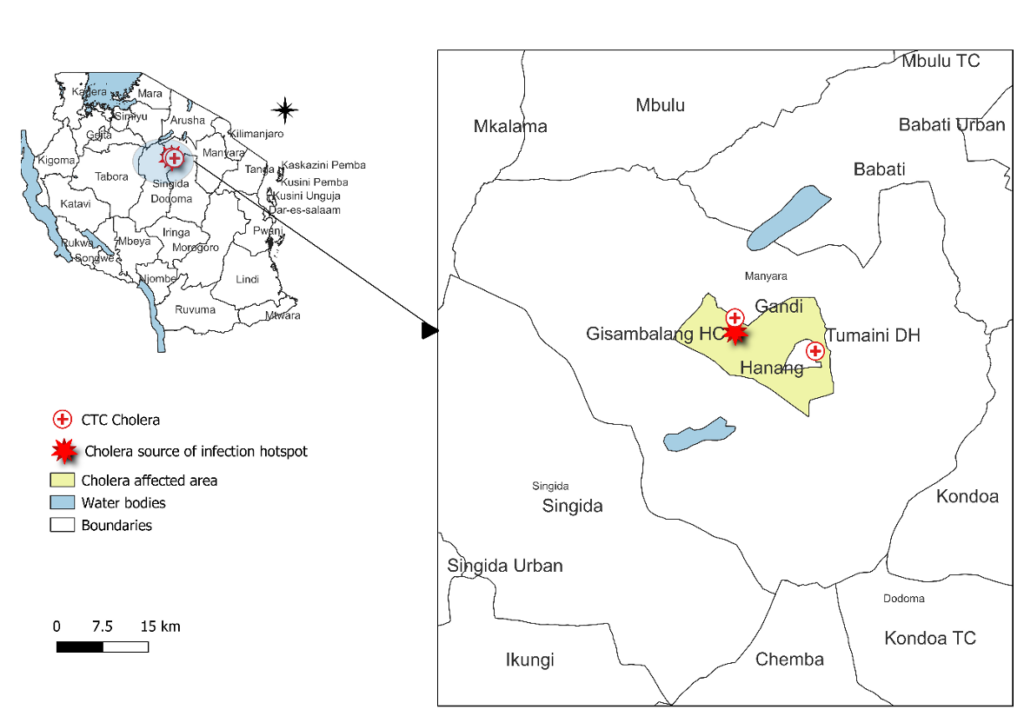
We conducted a descriptive analysis of the cholera cases recorded in the line list (from 08 to 18 July 2024) and performed an unmatched case-control study with a 1:1 case-control ratio to identify risk factors for cholera transmission. We selected one control per case due to resource limitations, such as time and funding. The cholera outbreak affected Hanang District in a ward called Gisambalang with a total population of 17,146 (Population 2022– Census) which is bordered by Kondoa and Chemba Councils. Hanang District is located in Manyara Region. This region has two rainy seasons, short rains from October to December and long rains from February to May. There is also the cold and dry season from June to September which causes drying of water sources leading to scarcity of water hence increasing the risk of cholera outbreak [4].
The response area was in Manyara Region located on the northern side of Tanzania with the regional capital as Babati. It is surrounded by Lake Manyara in the northern part of the region. It is bordered to the north by the Arusha Region, the northeast by Kilimanjaro Region, the east by Tanga Region, the south by Dodoma Region, the southeast by Morogoro Region, the southwest by Singida Region, and to the northwest by Simiyu Region. Manyara Region consists of 6 District Councils which are Babati, Babati Town, Hanang, Kiteto, Mbulu and Simanjiro. The highest mountain in the Manyara Region is Mount Hanang. The cholera affected ward was Gisambalang in Hanang District.
Based on this outbreak, we defined a suspected case of cholera as any person aged 2 years or older with acute watery diarrhoea and severe dehydration or who died from acute watery diarrhoea with no other known cause of death in Gisambalang ward from 8 to 26 July 2024. We also defined a confirmed case for this outbreak as any of the suspected cases in which V. cholerae was isolated from their specimen by culture.
Control was defined as any person aged five years and above living in Gisambalang Ward who had no history of diarrhea between July 8 and July 26, 2024 and lived in the same household as a line-listed cholera case.
Identification of cases and recruitment of controls
We obtained a line list of 86 suspected cases previously admitted at Gisambalang ward from the District Medical Officer. Sixty-one of these cases had stool samples tested with cholera rapid cholera diagnostic test (RDT) and 27 tested positive (44.3%). For the cases, we purposively selected all the 27 cholera RDT positive cases, 3 community deaths and randomly selected 15 of the 22 probable cases (were not subjected to RDT or culture) using simple random sampling by Microsoft Excel random number generator. Controls were selected within the case household. In the selected case household, all eligible members were listed and one member was selected randomly as a control for the case.
Laboratory Specimens Collected
Laboratory specimens were collected according to the National Guidelines for Prevention and Control of Cholera (3rd Edition, November 2015) to confirm the identity of the causative organism and test its antibiotic sensitivity. The guidelines specify that rectal swabs should be taken from the first 5 to 10 suspected cases during an outbreak for confirmation, and if any are positive, then every tenth case is sampled for further confirmation [5]. Currently, Tanzania utilizes Cholera Rapid Diagnostic Tests (RDTs) for suspected cholera cases to enable early detection of a probable outbreak, and for confirmation, rectal swabs are sent for culture testing to accurately isolation of Vibrio cholerae. Laboratory specimens collected included: Two stool samples per suspected case: one for cholera rapid diagnostic test screening and another for culture to confirm cholera, and water samples from the river and from tap water at Gisambalang ward. Tap water was cultured in alkaline peptone water and then sub cultured in TCBS media.
Sample size and Study Power Computation
For the case control study, we recruited 45 suspected line listed cases and 45 household controls giving a sample size of 90 participants. Considering eating outside as exposure for both cases and control 42.2% and 17.8% respectively at 95% confidence interval, the calculated power for this study was 72%. We selected only one control per case due to resource constraints including limited time for data collection and funding.
Hypothesis
Eating food prepared outside home was associated with being cholera case.
Information was obtained from the cholera line list at the beginning of the outbreak. All 45 recruited cases were visited at their homes. A standardized questionnaire [6] was used for data collection administered through face-to-face interviews using an electronic software (Kobo Toolbox). The questionnaire was used to collect information on social and demographic characteristics, history of illness and risk factors to both cases and controls. The data collection started from 22nd to 26th July 2024.
We visited a hotspot area and water samples (river and standing tap) were collected for Vibrio cholerae testing. We collected data from two affected hamlets in Gisambalang ward which are Gandi and Changanyikeni.
Data entry was done using Kobo Toolbox. The collected data was downloaded from Kobo Toolbox as an excel file and cleaned. The clean excel file was exported to Epi info 7 software version 7.2.5.0 for data analysis. Figures, bar charts and Epicurve were drawn using Microsoft excel. We conducted a descriptive analysis of the cholera cases recorded in the line list (from 08 to 18 July 2024) and performed an unmatched case-control study with a 1:1 case-control ratio to identify risk factors for cholera transmission. Additionally, QGIS 3.26.3 was used to map households visited and hotspot areas where water samples were taken. Binary Logistic regression was applied to assess factors associated with cholera disease transmission. The measure of association was the odds ratio with corresponding 95% confidence intervals. Statistical significance was set at a p-value of <0.05.
Ethical considerations
The study was conducted as part of an outbreak response which is one of the mandates of the Ministry of Health and did not require a formal review by an Ethical Review Committee. We obtained verbal consent from cases and controls before enrolment in the interview. Confidentiality of all the subjects was assured and maintained during and after the study. We anonymised the data before it was analysed to ensure patient confidentiality.
Results
Participant’s characteristics from line list
The line list contained 86 suspected cholera cases. We found an attack rate of (86/17146, 0.5%), also we found that the most affected age groups were those between 15 and 24 years old (17/86, 19.8%) and those aged 45+ years old (20/86, 23.3%). More than half of the cases (44/86, 51.2%) were female. A total of 79/86 (91.9%) cases were self-employed (farmers). A total of 85/86 (98.8%) were residing within Gisambalang ward, and 42/86 (48.8%) were from Gandi hamlet. A total of 82/86 (95.3%) were discharged, while 3 (3.5%) cases were reported as community deaths (Table 1).
Summary history of the index case
After analysing data from the line list, it was observed that the index case was recorded on 8 July 2024 at the Gisambalang ward in Gandi hamlet of Hanang district. The index case was an 18 year old female who had no history of travelling outside the district and region. She presented at Waranga Dispensary on 11 July 2024, was later transferred and admitted at Gisambalang HC on 12 July 2024. She had a history of using shallow well water from the river for domestic consumption without treating or boiling. She experienced acute watery diarrhoea, vomiting and dehydration. Vibrio cholerae was isolated from her stool. The two contacts from the index (the mother and a neighbour) who reported to have cared for the index case became sick and were confirmed cholera cases after Vibrio cholerae was isolated from their stool samples.
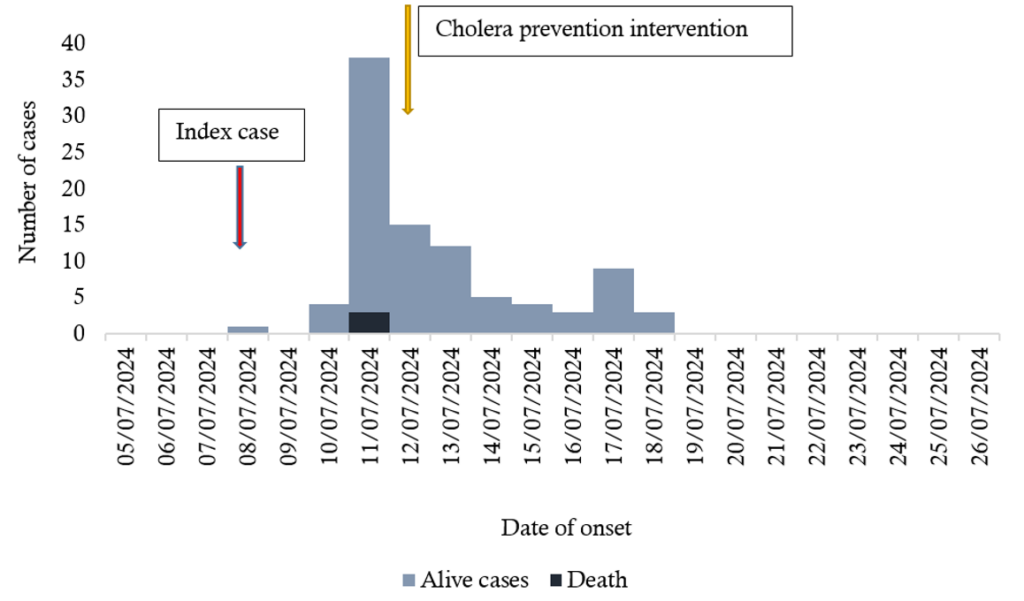
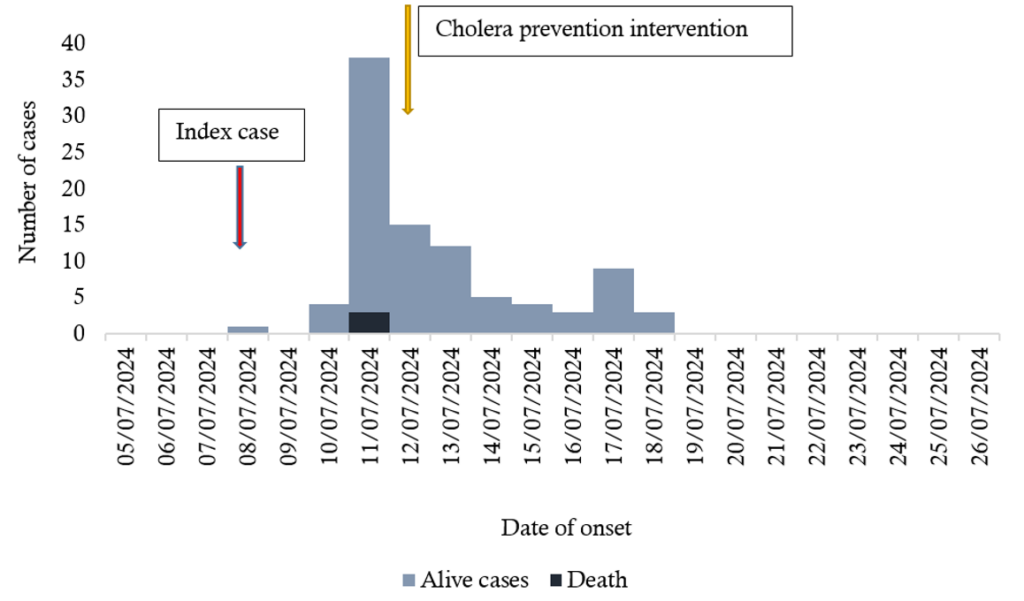
Affected population description
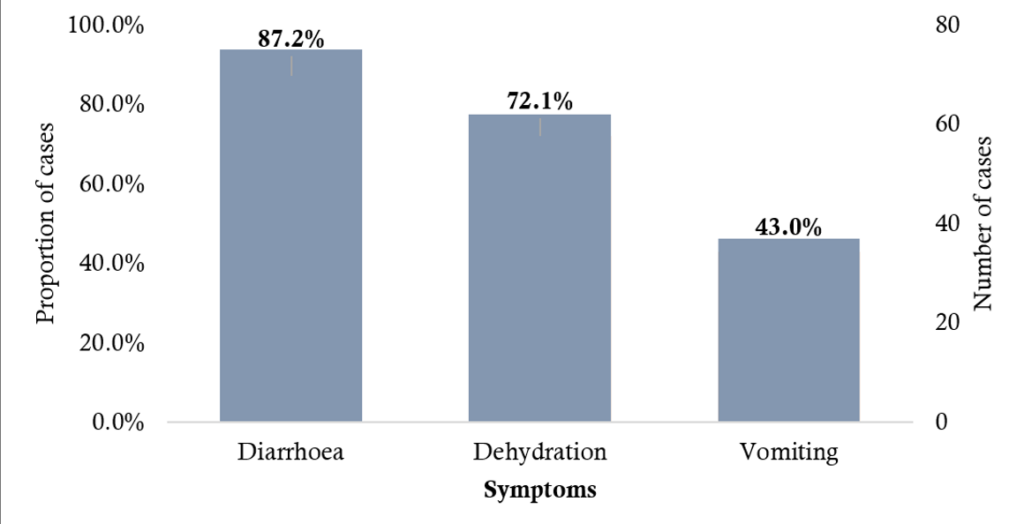
Person: Most of the cases had diarrhoea 75/86 (87.2%) followed by dehydration 62/86 (72.1%). Case fatality rate was 3/86 (3.5%) (Figure 1).
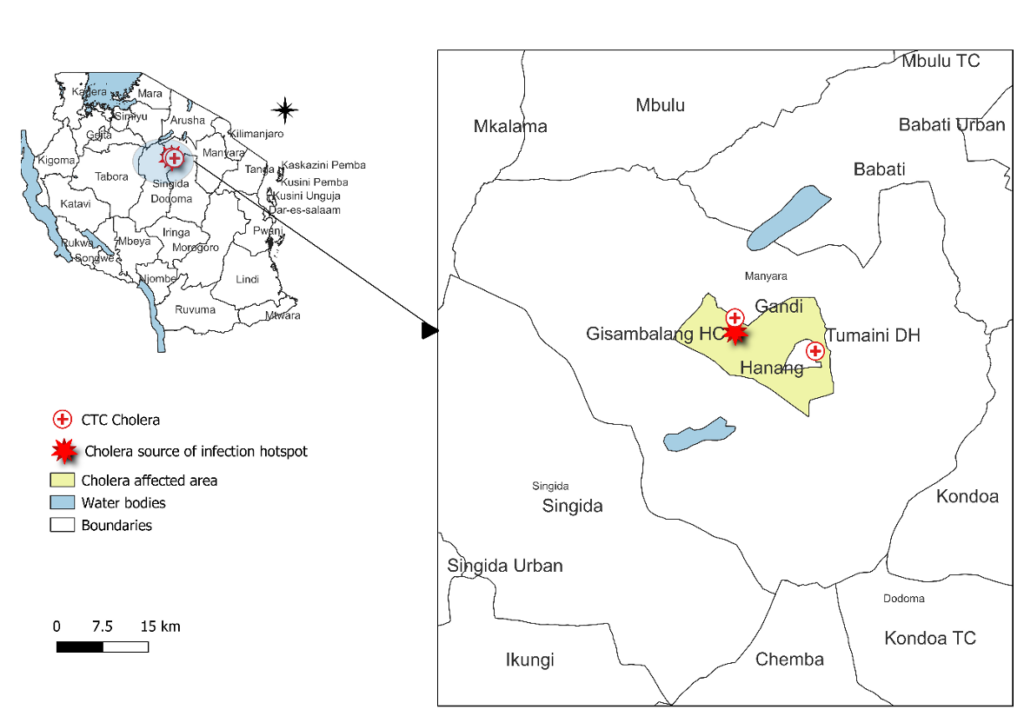
Spot map (Place): The cholera source of infection was found to be at Gandi hamlet where most cases were identified with a history of using water from shallow wells from the river for drinking and domestic purposes. The two centers for treatment and care were identified as Gisambalang Health Center and Tumaini District Hospital (Figure 2).
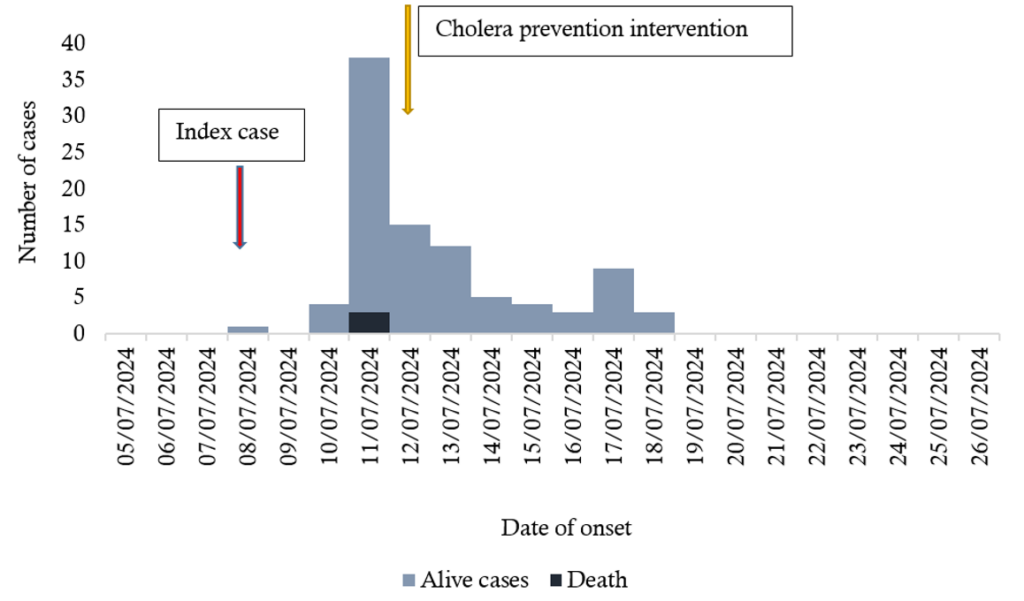
Epicurve (Time): A total of 86 cholera suspected cases were recorded including the index case. The first case recorded was on 8th July 2024 and more cases were seen on 11th July 2024 with a total of 39 live cases and 3 community deaths. The cholera response intervention started on 11th July 2024. Afterwards, there was decrease in the number of cases up to 18th July 2024. No case was reported since 19th July 2024. The case fatality rate was 3.5% (Figure 3).
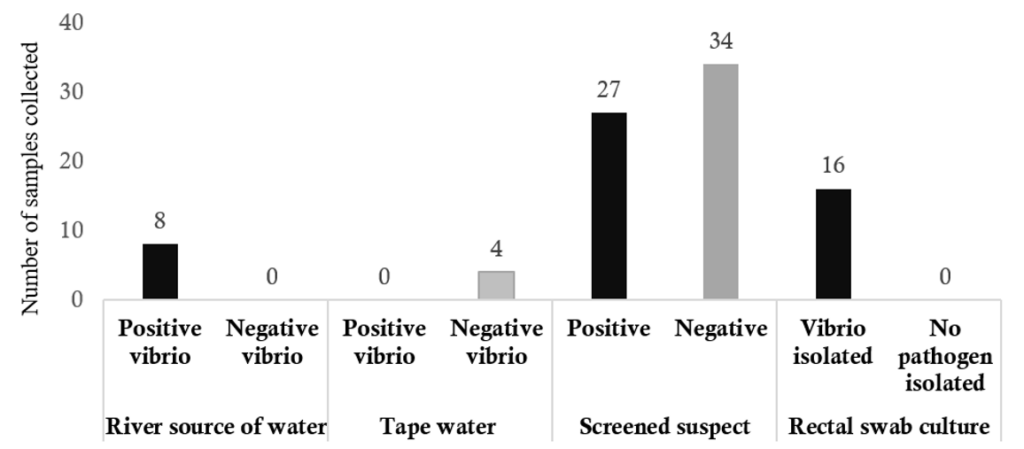
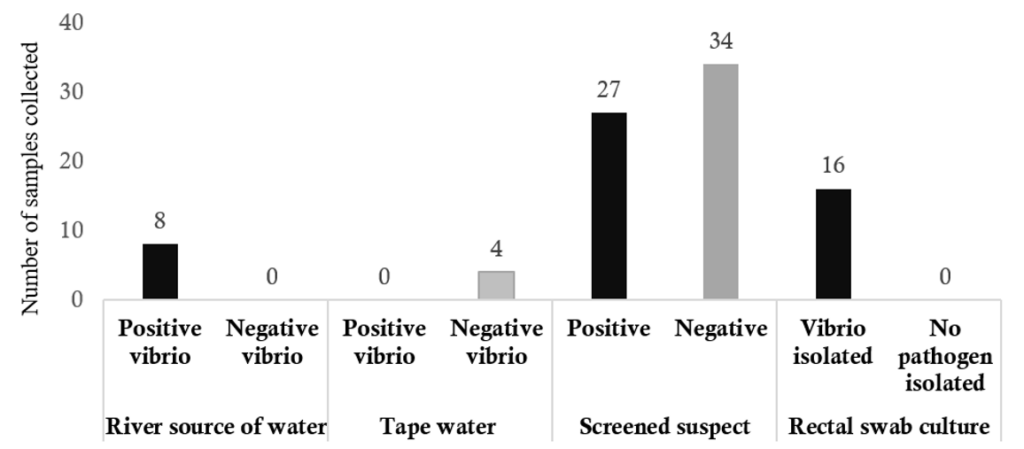
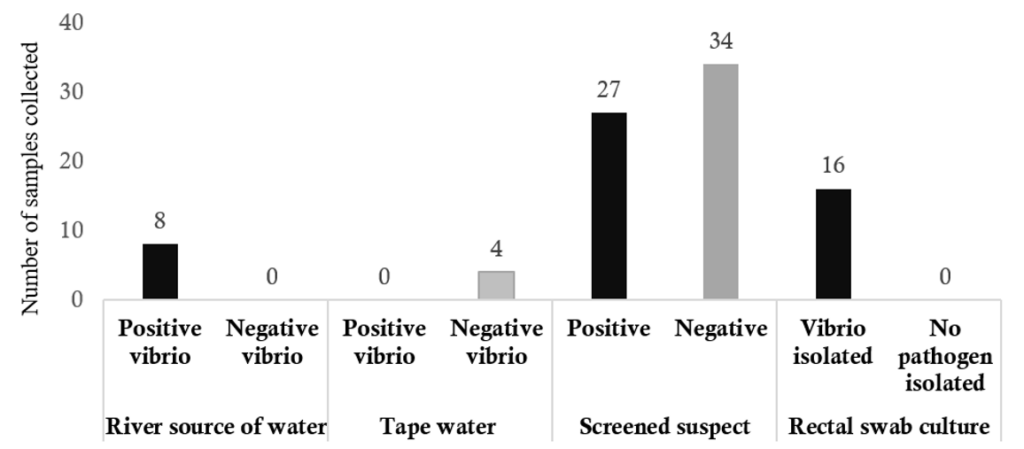
Laboratory results
Water source samples: A total of twelve (12) water samples comprising eight (8) from river and four (4) from tap water were taken. We found all eight (100%) samples from the river had Vibrio cholerae Ogawa serotype isolated and confirmed that the water source from the river were contaminated with the vibrio spp. No coliform was detected from all the four-tap water sources (Figure 4).
Testing of suspect cases: A total of 61/86 (70.9%) suspected cases had two stool samples taken for screening for cholera using cholera Rapid Diagnostic Test (RDT) and culture as they were presented to the health facility. The remaining 22/86 (25.6%) were classified as probable cholera cases based on case definition as there was stock out of cholera RDT and 3 (3.5%) community deaths occurred and were not tested. A total of 27/61 (44.3%) suspected cases were positive for cholera by RDT. Among the 27 probable cases tested positive by RDT, 16 (59.3%) cases were confirmed as cholera cases since Vibrio cholerae Ogawa serotype was isolated.
Etiological agent, source, risk factors and mode of transmission
From the laboratory findings the aetiology of the cholera outbreak at Gisambalang ward of Hanang district was Vibrio cholerae. The source of infection was the shallow wells from the river. Mode of transmission is the faecal oral route of the cholera cases.
Case control study participants characteristics
A total of 90 participant’s data was collected. Among them, 45 cases and 45 were controls. Majority of cholera cases were below 25 years 19/45 (42.2) than control 9/45 (20%). Almost half of the cases and controls were female 23/45(51.1%). We found out that 60.0% (27/45) of the cases and 75.6% (34/45) the controls were married. An equal number of cases and controls 32/45 (71.1%) had primary school level of education and 75.6% (34/45) cases were farmers compared to 91.2% (41/45) controls (Table 2).
Risk factors associated with cholera outbreak at Gisambalang ward
An unmatched case control study was carried out to evaluate the risk factors of cholera among cases and controls at Gisambalang ward. We found that individuals below the age of 25 years had 4.05 times the odds of getting cholera (AOR 4.05, 95%CI: 1.45-11.26) compared to those aged 25 plus years. Individuals who ate food mainly rice and ugali (cornmeal bread) outside their homes had 4.43 times the odds of getting cholera (AOR 4.43, 95%CI: 1.55- 12.63). We also found out that individuals who had contact with persons with symptoms of diarrhoea had 4.04 times odds of contracting cholera (AOR 4.04, 95%CI: 0.72- 22.78), however this was not statistically significant (Table 3).
Discussion
We found that most of the cholera cases were female, and more cases were between the age groups of 15- 24 years and those above 45 years. Nearly three quarter of cases reported using river water for domestic purposes and the most presented symptoms were diarrhoea and dehydration. The identified outbreak infection hotspot area was the river used as a source of drinking water and domestic purposes located at Gandi hamlet. The associated risk factors for the cholera outbreak was being below 25 years and eating outside home which included areas like, bars, neighbours, roadside, burial ceremony and food vendors.
We found that there were more cholera cases below 25 years of age than controls. This differs from the findings from the study done in Ethiopia [7] and this might be due to differences in the age distribution of the population affected by cholera in the two studies.
We found that the individuals below the age of 25 years were associated with contracting cholera. A similar study from Cameroon reported the same findings. This could be explained by younger individuals, particularly children and adolescents, more likely to engage in behaviours that increase exposure to contaminated water or food sources. Our study shows individuals in this age group at Gisambalang were involved in cattle rearing – an activity associated with poor personal hygiene and safe water access.
Furthermore, we found that females were mostly affected by cholera compared to males though this was not statistically significant. Several studies have reported the same findings [8,9]. However, another study done in Nigeria reported that males were more affected than females [10].
We found that the river was the probable source of cholera infection. This is consistent with the study done in Uganda in 2016 that revealed the contaminated river water was the source of infection [11]. This can be explained by the fact that residents of Gisambalang ward depend on river water as a source of drinking water and for domestic use as well as cattle’s rearing.
The current outbreak most likely resulted from a common source infection which was the contaminated water from the river, as the index case reported used the river water for drinking and domestic purposes. The two contacts from the index (the mother and neighbour) reported to have cared for the index case and were confirmed cholera positive with Vibrio cholerae isolated from their stool samples. This could probably indicate that the disease was transmitted from common source. Therefore removing the source of infection can result in controlling the transmission [12]. Furthermore, the epi-curve revealed that there was a gradual decrease in cases till this reporting period. This could be due to the immediate public health interventions which includes community-wide dissemination of health messages focusing on sanitation and proper use of latrines, distribution of aqua tabs for water treatment, distribution of tap water, stopping the use of river water and practicing personal hygiene.
However, there was no statistically significant association between river water use and cholera infection in our study. This is probably because we used household controls; a case and household control share the same domestic water source which likely cancelled out the association.
The case fatality rate recorded in this study was 3.5%. The findings were lower than those from similar studies done in Nigeria which revealed a 4.1% and 6% case fatality rates respectively [9,13]. Our findings however were higher compared to the study done in Mwanza, Tanzania [14]. The higher case fatality reported in our study could probably be explained by delayed notification of the outbreak leading to the late arrival of the response team at the district level, which may have contributed to ineffective case management by local responders during the early stages of the outbreak [9]. The district responding team in our study arrived at the affected area and started responding to the outbreak almost four days later after the recorded index case. The delay time of response was further explained by the study which evaluated seventy-six outbreaks from 34 countries which found the median time of delays from symptom onset of the primary case to case presentation and to response were 5 days and 10 days respectively, result in large clusters of infection that was difficult to contain [15].
We identified that eating outside home was a risk factor for cholera infection in this outbreak consistent with our study hypothesis. We found that individuals who ate outside home had four times the odds of contracting cholera. This could be explained by roadside food vendors who did not meet minimum food hygiene standards being a potential source of cholera infection. Our results were similar to several studies that revealed eating street foods were associated with cholera transmission, indicating that interventions directed at street food vendors including emphasis on safe food handling, proper hygiene practices and the importance of using clean water for food preparation may be an important pathway to interrupt transmission during an outbreak [16–19]. Regulation or a ban on roadside food vending will help to stop the infection.
The limitations encountered in our outbreak investigation and response include; first, the recall bias by participants when answering interview questions which could have distorted the reliability of the collected data. Secondly, we used household controls which potentially led to shared environmental and socio-behavioural factors among cases and controls, reducing the likelihood of detecting independent associations between these shared exposures and outcome. Third, household members often have similar lifestyles, socioeconomic conditions, and access to healthcare, leading to a lack of variability in key exposure factors, this may introduce bias and limit the generalizability of findings. Fourth, there might be misclassification of cases as not all cases included in the study were confirmed by culture. Lastly, the small sample size used had a statistical power of 72% which could have limited our study’s ability to detect the true effect hence inaccurate conclusions.
Conclusion
Overall, the cholera outbreak in Hanang district, specifically in Gisambalang ward, affected farmers. Also the case fatality rate was high, 3.5%. The age below 25 years and eating outside home was significantly associated with cholera transmission.
We recommend to the Council Health Management Team (CHMT) to emphasis on early intervention in targeted public health education, personal hygiene and sanitation. For the Rural Water Supply and Sanitation Agency (RUWASA) we recommend on safe water supply, improved water treatment. District Health Officer to advocate food safety regulations.
What is already known about the topic
- Cholera is a contagious diarrhea disease caused by Vibrio cholerae that is transmitted via the fecal oral route
- The symptom is frequent amounts of watery diarrhea lasting a few days. Vomiting and muscle cramps may also occur
- Diarrhea can be so severe that leads within hours to severe dehydration and electrolyte imbalance
What this study adds
- The risk factors for the outbreak at Gisambalang ward was being young age group (below 25 years) and eating outside home which was significantly associated with the cholera transmission
Funding
This work has been supported by the United States President’s Emergency Plan for Aids Relief (PEPFAR) through the Centre of Excellence in Health Monitoring and Evaluation, Mzumbe University under the Centre for Disease Control and Prevention (CDC), Project Cooperative Agreement No: “NU2GGH002292”
Acknowledgements
We express our gratitude to the office of the Regional Medical Officer in Manyara region and the District Medical Officers of Hanang District for their cooperation and hard work in supporting the cholera outbreak investigation and response. We also acknowledge the technical and financial support provided by CDC/PEPFAR through Mzumbe University for this activity, and the support from the TFELTP program for the logistics arrangement.
| Characteristics | Frequency | Proportion (%) |
|---|---|---|
| Age group (years) | ||
| <5 | 16 | 18.6 |
| 5–14 | 11 | 12.8 |
| 15–24 | 17 | 19.8 |
| 25–34 | 14 | 16.3 |
| 35–44 | 8 | 9.3 |
| ≥45 | 20 | 23.3 |
| Median 24 (IQR; 8–41) | ||
| Sex | ||
| Female | 44 | 51.2 |
| Male | 42 | 48.8 |
| Occupation | ||
| Self employed | 79 | 91.9 |
| Unemployed | 7 | 8.1 |
| Ward | ||
| Gisambalang | 85 | 98.8 |
| Dirma | 1 | 1.2 |
| Hamlet | ||
| Gandi | 42 | 48.8 |
| Changanyikeni | 22 | 25.6 |
| Gisambalang | 13 | 15.1 |
| Waranga | 3 | 3.5 |
| Masusu | 2 | 2.3 |
| Gobanga | 1 | 1.2 |
| Kibaoni | 1 | 1.2 |
| Kilomita 5 | 1 | 1.2 |
| Masaha | 1 | 1.2 |
| Mitiriangu/Kondoa | 1 | 1.2 |
| Attended HF | ||
| Yes | 83 | 96.5 |
| No | 3 | 3.5 |
| Admitted | ||
| Yes | 72 | 83.7 |
| No | 14 | 16.3 |
| Final outcome | ||
| Discharged | 82 | 95.3 |
| Died | 3 | 3.5 |
| Still sick | 1 | 1.2 |
| Place of death | ||
| Community | 3 | 100.0 |
| Health facility | 0 | 0.0 |
| Demographic factors | Cholera case (N=45) n (%) | Control (N=45) n (%) |
|---|---|---|
| Age (years) | ||
| <25 | 19 (42.2) | 9 (20.0) |
| ≥25 | 26 (57.8) | 36 (80.0) |
| Median age | 28 (IQR: 18–42) | 34 (IQR: 26–50) |
| Gender | ||
| Male | 22 (48.9) | 22 (48.9) |
| Female | 23 (51.1) | 23 (51.1) |
| Marital status | ||
| Married | 27 (60) | 34 (75.6) |
| Single | 16 (35.6) | 7 (15.6) |
| Divorced | 1 (2.2) | 1 (2.2) |
| Widowed | 1 (2.2) | 3 (6.7) |
| Education Level | ||
| Not attended school | 13 (28.9) | 12 (26.7) |
| Primary | 32 (71.1) | 32 (71.1) |
| Secondary | 0 (0) | 1 (2.2) |
| Tertiary | ||
| Occupation | ||
| Farmer | 34 (75.6) | 41 (91.2) |
| Pupil or Student | 2 (4.4) | 2 (4.4) |
| Child | 9 (20.0) | 1 (2.2) |
| Businessman/woman | 0 (0) | 1 (2.2) |
| Risk factors | Cholera case (n=45) n (%) |
Control (n=45) n (%) |
Crude Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|
| Age (years) | ||||
| <25 | 19 (42.2) | 9 (20.0) | 2.92 (1.14–7.48) | 4.05 (1.45–11.26) |
| ≥25 | 26 (57.8) | 36 (80.0) | Ref | Ref |
| Sex | ||||
| Male | 22 (48.9) | 22 (48.9) | 1.0 (0.44–2.29) | 0.94 (0.40–2.20) |
| Female | 23 (51.1) | 23 (51.1) | Ref | Ref |
| Contact with patients with symptoms of diarrhoea | ||||
| Yes | 5 (11.1) | 2 (4.4) | 2.69 (0.49–14.62) | 4.04 (0.72–22.78) |
| No | 40 (88.9) | 43 (95.6) | Ref | Ref |
| Individual eaten outside home (last 5 days) | ||||
| Yes | 19 (42.2) | 8 (17.8) | 3.38 (1.29–8.88) | 4.43 (1.55–12.63) |
| No | 26 (57.8) | 37 (82.2) | Ref | Ref |
| Source of domestic water | ||||
| River | 32 (71.1) | 33 (73.3) | 1.26 (0.46–3.43) | 1.38 (0.48–3.95) |
| Shallow wells | 2 (4.4) | 1 (2.2) | 2.44 (0.19–31.53) | 2.79 (0.20–38.71) |
| Tap water | 9 (20.0) | 11 (24.4) | Ref | Ref |
References
- World Health Organization. Cholera [Internet]. Geneva: World Health Organization; 2024 Dec 5 [cited 2025 May 20]. Available from: https://www.who.int/news-room/fact-sheets/detail/cholera.
- United Nations. WHO reports exponential rise in cholera cases in Africa. UN News [Internet]. New York: United Nations; 2023 Feb 9 [cited 2025 May 20]. Available from: https.com/en/story/2023/02/1133337.
- World Health Organization. Multi-country outbreak of cholera: External Situation Report no. 13 [Internet]. Geneva: World Health Organization; 2024 Apr 17 [cited 2025 May 20]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20240417_multi-country_outbreak-of-cholera_sitrep_-13.pdf?sfvrsn=90f742ae_3.
- Charnley GEC, Kelman I, Murray KA. Drought-related cholera outbreaks in Africa and the implications for climate change: a narrative review. Pathog Glob Health. 2022;116(1):3-12. Available from: https://www.tandfonline.com/doi/full/10.1080/20477724.2021.1981716. doi:10.1080/20477724.2021.1981716.
- Ministry of Health, Community Development, Gender, Seniors and Children (Tanzania). National guidelines for prevention and control of cholera. 3rd ed. Dar es Salaam: Ministry of Health, Community Development, Gender, Seniors and Children; 2015.
- Global Taskforce on Cholera Control. Public health surveillance for cholera: guidance document 2024 [Internet]. Geneva: Global Taskforce on Cholera Control; 2024 [cited 2025 May 20]. Available from: https://www.gtfcc.org/wp-content/uploads/2024/04/public-health-surveillance-for-cholera-guidance-document-2024.pdf.
- Dinede G, Abagero A, Tolosa T. Cholera outbreak in Addis Ababa, Ethiopia: a case-control study. PLoS One. 2020;15(7):e0235440. Yahav D, editor. Available from: https://dx.plos.org/10.1371/journal.pone.0235440. doi:10.1371/journal.pone.0235440.
- Ibrahim BS, Mohammed Y, Usman R, Okon UA, Katchy UI, Olufemi AA, Niyang M, Gobir B, Okunromade OF. Outbreak of cholera at Dutsen-Abba Ward Zaria local government area, Kaduna State Nigeria 2015: the importance of hygienic practices. Int J Community Med Public Health. 2017;4(5):1473-1479. Available from: http://www.ijcmph.com/index.php/ijcmph/article/view/1174. doi:10.18203/2394-6040.ijcmph20171757.
- Gidado S, Awosanya E, Haladu S, Ayanleke HB, Idris S, Mamuda I, Mohammed A, Akataobi CI, Waziri NE, Nguku P. Cholera outbreak in a naïve rural community in Northern Nigeria: the importance of hand washing with soap, September 2010. Pan Afr Med J. 2018;30:5. Available from: http://www.panafrican-med-journal.com/content/article/30/5/full/. doi:10.11604/pamj.2018.30.5.12768.
- Elimian KO, Musah A, Mezue S, Oyebanji O, Yennan S, Jinadu A, Williams N, Ogunleye A, Fall IS, Yao M, Eteng WE, Abok P, Popoola M, Chukwuji M, Omar LH, Ekeng E, Balde T, Mamadu I, Adeyemo A, Namara G, Okudo I, Alemu W, Peter C, Ihekweazu C. Descriptive epidemiology of cholera outbreak in Nigeria, January-November, 2018: implications for the global roadmap strategy. BMC Public Health. 2019;19(1):1264. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7559-6. doi:10.1186/s12889-019-7559-6.
- Okello PE, Bulage L, Riolexus AA, Kadobera D, Kwesiga B, Kajumbula H, Mulongo M, Namboozo EJ, Pimundu G, Ssewanyana I, Kiyaga C, Aisu S, Zhu BP. A cholera outbreak caused by drinking contaminated river water, Bulambuli District, Eastern Uganda, March 2016. BMC Infect Dis. 2019;19(1):516. Available from: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-4036-x. doi:10.1186/s12879-019-4036-x.
- Public Health Agency of Canada. Epidemic Curves [Internet]. Ontario: Public Health Agency of Canada; [cited 2024 Jul 26]. Available from: https://sphweb.bumc.bu.edu/otlt/MPH-Modules/EP/EP713_DescriptiveEpi/EP713_DescriptiveEpi3.html.
- Dalhat MM, Isa AN, Nguku P, Nasir SG, Urban K, Abdulaziz M, Dankoli RS, Nsubuga P, Poggensee G. Descriptive characterization of the 2010 cholera outbreak in Nigeria. BMC Public Health. 2014;14(1):1167. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-14-1167. doi:10.1186/1471-2458-14-1167.
- Madullu MT, Thomas DSK, Nyanza EC, Seni J, Ngallaba SE, Kiluvia S, Asori M, Kangmennaang J. Spatial distribution of suspected and confirmed cholera cases in Mwanza City, Northern Tanzania. PLOS Glob Public Health. 2023;3(1):e0001261. Available from: https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0001261. doi:10.1371/journal.pgph.0001261.
- Ratnayake R, Finger F, Edmunds WJ, Checchi F. Early detection of cholera epidemics to support control in fragile states: estimation of delays and potential epidemic sizes. BMC Med. 2020;18(1):397. Available from: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-020-01865-7. doi:10.1186/s12916-020-01865-7.
- Nsagha DS, Atashili J, Fon PN, Tanue EA, Ayima CW, Kibu OD. Assessing the risk factors of cholera epidemic in the Buea Health District of Cameroon. BMC Public Health. 2015;15(1):1128. Available from: http://www.biomedcentral.com/1471-2458/15/1128. doi:10.1186/s12889-015-2485-8.
- Richterman A, Sainvilien DR, Eberly L, Ivers LC. Individual and household risk factors for symptomatic cholera infection: a systematic review and meta-analysis. J Infect Dis. 2018;218(suppl_3):S154-S164. Available from: https://academic.oup.com/jid/article/218/suppl_3/S154/5076163. doi:10.1093/infdis/jiy444.
- Grandesso F, Allan M, Jean-Simon PSJ, Boncy J, Blake A, Pierre R, Alberti KP, Munger A, Elder G, Olson D, Porten K, Luquero FJ. Risk factors for cholera transmission in Haiti during inter-peak periods: insights to improve current control strategies from two case-control studies. Epidemiol Infect. 2014;142(8):1625-1635. Available from: https://www.cambridge.org/core/product/identifier/S0950268813002562/type/journal_article. doi:10.1017/S0950268813002562.
- Cummings MJ, Wamala JF, Eyura M, Malimbo M, Omeke ME, Mayer D, Lukwago L. A cholera outbreak among semi-nomadic pastoralists in North Eastern Uganda: epidemiology and interventions. Epidemiol Infect. 2012;140(8):1376-1385. Available from: https://www.cambridge.org/core/product/identifier/S0950268811001956/type/journal_article. doi:10.1017/S0950268811001956.
Menu, Tables and Figures
Navigate this article
Tables
| Characteristics | Frequency | Proportion (%) |
|---|---|---|
| Age group (years) | ||
| <5 | 16 | 18.6 |
| 5–14 | 11 | 12.8 |
| 15–24 | 17 | 19.8 |
| 25–34 | 14 | 16.3 |
| 35–44 | 8 | 9.3 |
| ≥45 | 20 | 23.3 |
| Median 24 (IQR; 8–41) | ||
| Sex | ||
| Female | 44 | 51.2 |
| Male | 42 | 48.8 |
| Occupation | ||
| Self employed | 79 | 91.9 |
| Unemployed | 7 | 8.1 |
| Ward | ||
| Gisambalang | 85 | 98.8 |
| Dirma | 1 | 1.2 |
| Hamlet | ||
| Gandi | 42 | 48.8 |
| Changanyikeni | 22 | 25.6 |
| Gisambalang | 13 | 15.1 |
| Waranga | 3 | 3.5 |
| Masusu | 2 | 2.3 |
| Gobanga | 1 | 1.2 |
| Kibaoni | 1 | 1.2 |
| Kilomita 5 | 1 | 1.2 |
| Masaha | 1 | 1.2 |
| Mitiriangu/Kondoa | 1 | 1.2 |
| Attended HF | ||
| Yes | 83 | 96.5 |
| No | 3 | 3.5 |
| Admitted | ||
| Yes | 72 | 83.7 |
| No | 14 | 16.3 |
| Final outcome | ||
| Discharged | 82 | 95.3 |
| Died | 3 | 3.5 |
| Still sick | 1 | 1.2 |
| Place of death | ||
| Community | 3 | 100.0 |
| Health facility | 0 | 0.0 |
Table 1. Socio-demographic characteristics of suspected cholera cases at Gisambalang ward July 2024, N=86
| Demographic factors | Cholera case (N=45) n (%) | Control (N=45) n (%) |
|---|---|---|
| Age (years) | ||
| <25 | 19 (42.2) | 9 (20.0) |
| ≥25 | 26 (57.8) | 36 (80.0) |
| Median age | 28 (IQR: 18–42) | 34 (IQR: 26–50) |
| Gender | ||
| Male | 22 (48.9) | 22 (48.9) |
| Female | 23 (51.1) | 23 (51.1) |
| Marital status | ||
| Married | 27 (60) | 34 (75.6) |
| Single | 16 (35.6) | 7 (15.6) |
| Divorced | 1 (2.2) | 1 (2.2) |
| Widowed | 1 (2.2) | 3 (6.7) |
| Education Level | ||
| Not attended school | 13 (28.9) | 12 (26.7) |
| Primary | 32 (71.1) | 32 (71.1) |
| Secondary | 0 (0) | 1 (2.2) |
| Tertiary | ||
| Occupation | ||
| Farmer | 34 (75.6) | 41 (91.2) |
| Pupil or Student | 2 (4.4) | 2 (4.4) |
| Child | 9 (20.0) | 1 (2.2) |
| Businessman/woman | 0 (0) | 1 (2.2) |
Table 2. Socio-demographic characteristics of case-control study participants, Gisambalang ward July 2024
| Risk factors | Cholera case (n=45) n (%) | Control (n=45) n (%) | Crude Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|
| Age (years) | ||||
| <25 | 19 (42.2) | 9 (20.0) | 2.92 (1.14–7.48) | 4.05 (1.45–11.26) |
| ≥25 | 26 (57.8) | 36 (80.0) | Ref | Ref |
| Sex | ||||
| Male | 22 (48.9) | 22 (48.9) | 1.0 (0.44–2.29) | 0.94 (0.40–2.20) |
| Female | 23 (51.1) | 23 (51.1) | Ref | Ref |
| Contact with patients with symptoms of diarrhoea | ||||
| Yes | 5 (11.1) | 2 (4.4) | 2.69 (0.49–14.62) | 4.04 (0.72–22.78) |
| No | 40 (88.9) | 43 (95.6) | Ref | Ref |
| Individual eaten outside home (last 5 days) | ||||
| Yes | 19 (42.2) | 8 (17.8) | 3.38 (1.29–8.88) | 4.43 (1.55–12.63) |
| No | 26 (57.8) | 37 (82.2) | Ref | Ref |
| Source of domestic water | ||||
| River | 32 (71.1) | 33 (73.3) | 1.26 (0.46–3.43) | 1.38 (0.48–3.95) |
| Shallow wells | 2 (4.4) | 1 (2.2) | 2.44 (0.19–31.53) | 2.79 (0.20–38.71) |
| Tap water | 9 (20.0) | 11 (24.4) | Ref | Ref |
Table 3. The associated risk factors of cholera outbreak at Gisambalang ward July 2024
Figures
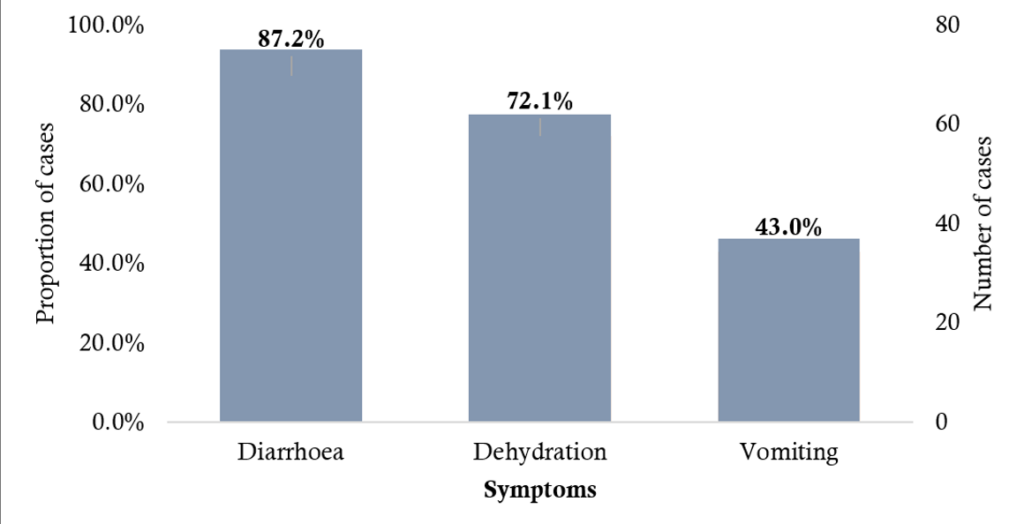
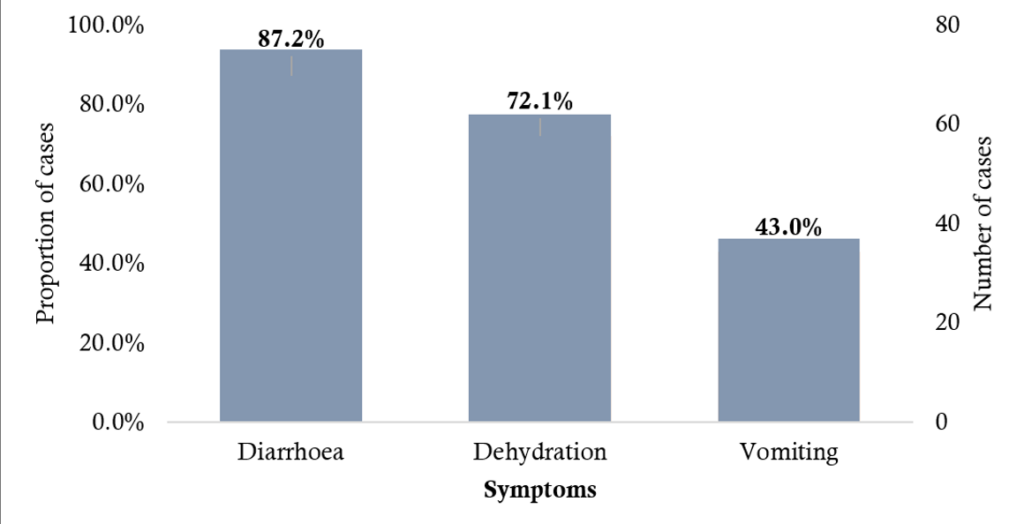
Figure 1. Distribution of cholera symptoms among cases at Gisambalang ward July 2024
Keywords
- Tanzania
- Manyara
- Cholera outbreak
- Hanang
