Research | Open Access | Volume 8 (4): Article 89 | Published: 07 Nov 2025
Evaluation of the malaria death notification surveillance system focusing on the electronic malaria death investigation form piloted in Manicaland Province, Zimbabwe, 2023
Menu, Tables and Figures
Navigate this article
Tables
| Cadre of health worker | Excellent | Good | Fair | Poor | Total |
|---|---|---|---|---|---|
| Doctors | 0 | 0 | 0 | 4 | 4 |
| Nurses | 4 | 10 | 11 | 0 | 25 |
| HIOs | 7 | 6 | 0 | 0 | 13 |
| HIAs | 1 | 9 | 2 | 0 | 12 |
| DECs | 1 | 4 | 1 | 0 | 6 |
| Records clerks | 0 | 1 | 1 | 0 | 2 |
Table 1: Knowledge level of study participants on the electronic malaria death notification surveillance system, Manicaland, Zimbabwe, 2023, N=62
| Time taken to submit the electronic form | Frequency (%) |
|---|---|
| 24 hours | 4 (6) |
| Within 7 days | 31 (50) |
| Within 2 weeks | 21 (34) |
| More than 2 weeks | 6 (10) |
Table 2: Time taken to notify a malaria death electronically in Manicaland, Zimbabwe, 2023
| Key Finding | Recommendation | Responsible person | Timeline |
|---|---|---|---|
| Delayed submission of paper-based forms due to delay by doctors to complete their section on the form. | • To have guidelines which clearly stipulate the timelines • Doctors or nurses who attended the deceased should complete the form as a team as soon as the death occurs • Phase out the paper-based forms in Manicaland | NMCP District Medical Officer (DMO) and District Nursing Officer (DNO) NMCP | 01-06-24 Immediately 01-06-24 |
| Fifteen out of 50 (30%) of the reviewed forms had incompletely filled forms. | • Put required fields on the form | NMCP Data manager | 09-02-24 |
| Poor knowledge of the electronic system was mainly among doctors and nurses. | • Malaria death notification trainings should include doctors and nurses • Malaria electronic death notification should be assessed during quarterly support and supervision | Provincial Medical Director (PMD) | 15-02-24 Immediately |
| Fields on the electronic form are not in sequence and the field for age does not accommodate age less than 1. | Revise the electronic form | NMCP- Data manager | 05-02-24 |
| Inadequate airtime | Include airtime for Health Information Officers in the hospital budgets | DMO | 15-02-24 |
Table 3: Recommendations to improve electronic malaria death surveillance system, Manicaland, Zimbabwe, 2023
Figures
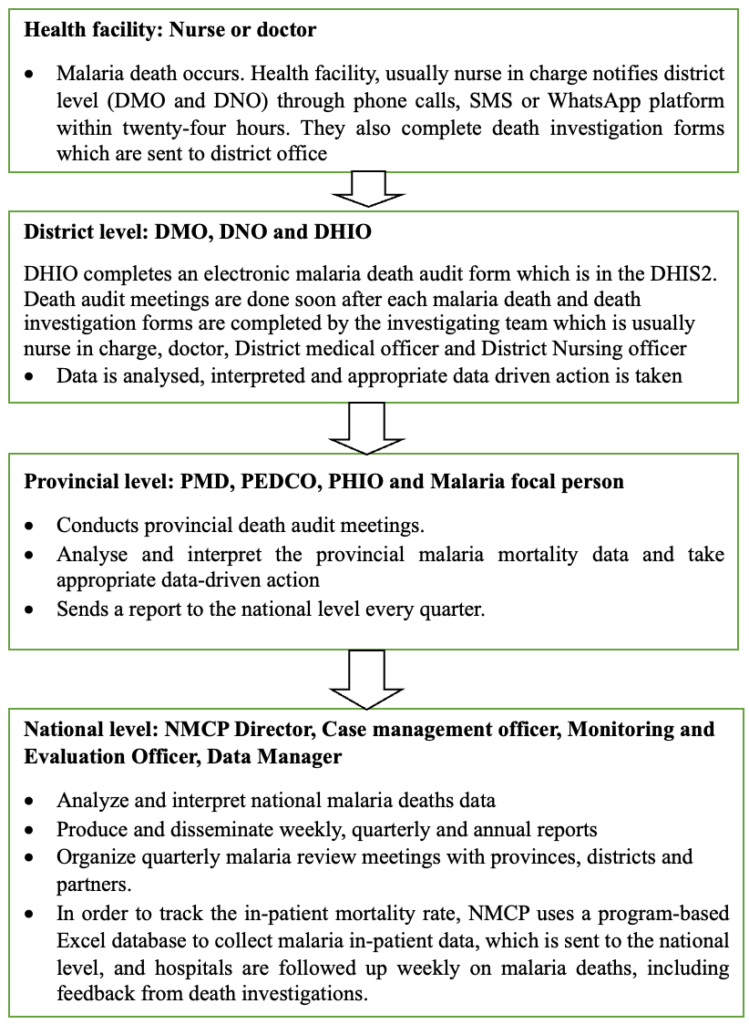
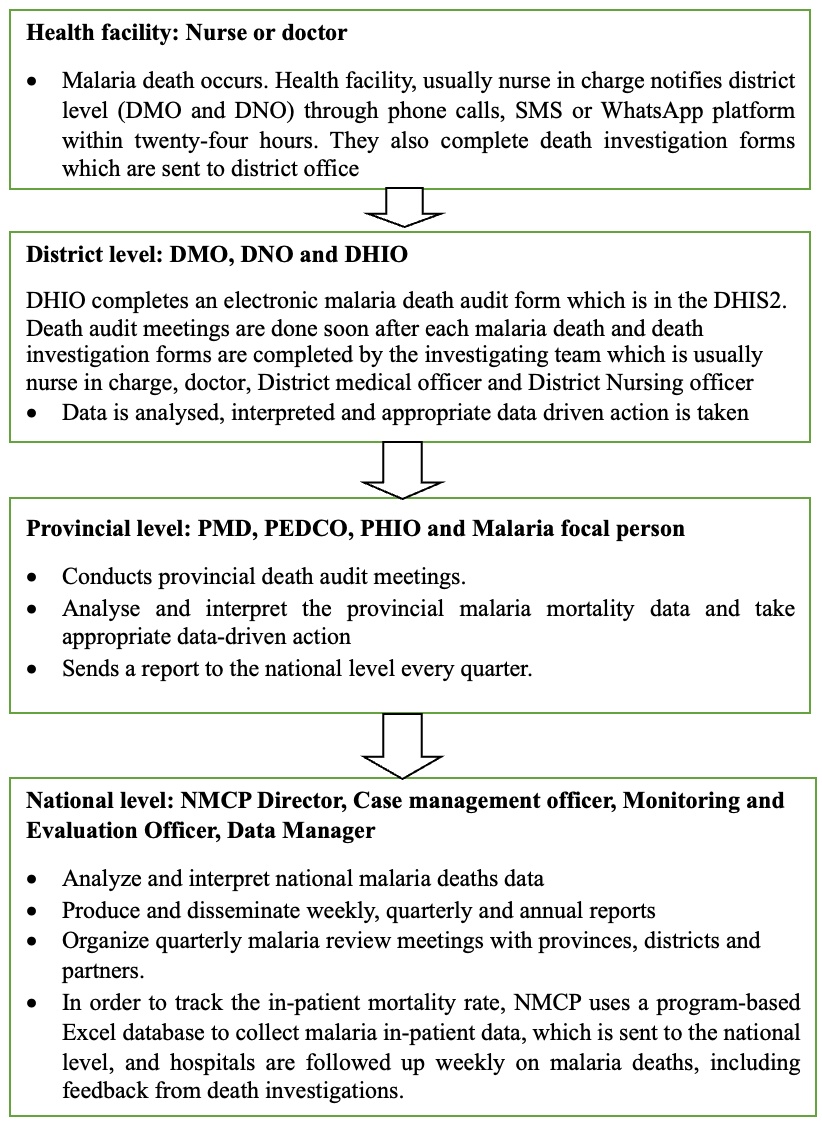
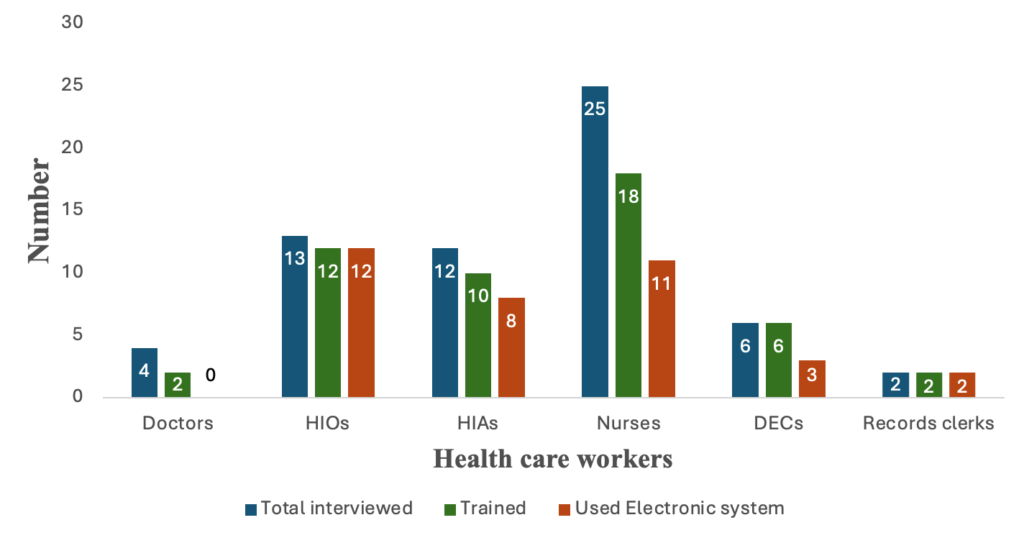
Figure 2: Distribution of mumps attack rates by district, Western North Region, August 2022
Keywords
- Malaria
- Death
- Electronic
- Surveillance
- Investigation
Delight Mhungira1, Patience Dhliwayo2, Addmore Chadambuka3, Tsitsi Juru3, Gerald Shambira1, Notion Gombe4, Gibson Mandozana1, Mufuta Tshimanga1
1University of Zimbabwe, Department of Global Public Health and Family Medicine, Harare, Zimbabwe, 2National Malaria Control Program, Harare, Zimbabwe, 3Zimbabwe Field Epidemiology Training Program, Harare, Zimbabwe, 4African Field Epidemiology Network, Harare, Zimbabwe
&Corresponding author: Addmore Chadambuka, Zimbabwe Field Epidemiology Training Program, 68 Kaguvi Building, Cnr 4th/Central Avenue, Harare, Zimbabwe, Email: achadambuka1@yahoo.co.uk, ORCID: https://orcid.org/0000-0003-2407-1172
Received: 06 Dec 2024, Accepted: 06 Nov 2025, Published: 07 Nov 2025
Domain: Field Epidemiology
Keywords: Malaria, Death, Electronic, Surveillance, Investigation
©Delight Mhungira et al. Journal of Interventional Epidemiology and Public Health (ISSN: 2664-2824). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Delight Mhungira et al., Evaluation of the malaria death notification surveillance system focusing on the electronic malaria death investigation form piloted in Manicaland Province, Zimbabwe, 2023. Journal of Interventional Epidemiology and Public Health. 2025;8(4):89. https://doi.org/10.37432/jieph-d-24-02009
Abstract
Introduction: Zimbabwe is accelerating towards malaria elimination by 2030. Investigation of malaria deaths is a requirement. The malaria case management technical working group recommended the development of an electronic malaria death investigation form after noting the challenges of the paper-based one. The form was piloted in Manicaland in 2022. We evaluated it to assess if it could be rolled out to other provinces. We evaluated the electronic malaria death notification surveillance system in Manicaland province, 2023.
Methods: A descriptive cross-sectional study using the updated CDC guidelines for evaluating public health surveillance systems was conducted at 11 hospitals in Manicaland. Administered 62 questionnaires among healthcare workers (HCWs). Conducted key informant interviews and reviewed records. We generated frequencies, means, and proportions using Epi Info 7.2.5.
Results: The median age for participants was 31 (IQR: 25-39). Their median year in service was 9 (IQR: 2-6). Out of 18 trained nurses, seven had not used the system. No trained doctors had used the system, and 40% of HCWs said the electronic form excluded zero reporting and private sector participation. 80% found the form easy to use, 20% found it confusing, and 50% notified deaths electronically within 24 hours. There were no guidelines. The estimated once-off cost of running the system per district per year was USD 3,000.
Conclusion: The system was simple, flexible, acceptable and useful. However, it was poor on timeliness, sensitivity and representativeness and data from the private health facilities.
Introduction
Malaria death notification surveillance is the ongoing, systematic collection, analysis and interpretation of malaria-related data, and the use of that data in the planning, implementation and evaluation of public health practice. [1] Data pertaining to malaria deaths helps the Ministry of Health and Child Care to monitor changing disease mortality patterns, their determinants and frequencies. It also helps in designing effective health interventions and evaluating the impact of malaria control programmes. [2]
In Zimbabwe, malaria deaths are investigated using malaria death investigation forms which were introduced by the Ministry of Health and Child Care (MoHCC) in 2011. These are physical documents which are completed in triplicate, for every malaria death, within 7 days and copies are submitted to the local health information department, district health information office and the National Malaria Control Programme (NMCP). The death investigation form has three pages and five sections which capture demographics, details of patient’s visit to first facility, treatment at secondary level, treatment at tertiary level and complications observed. The information is used to inform malaria case management guidelines and patient care protocols.
In 2021, the case management technical working group at the NMCP recommended the development of an electronic malaria death reporting system after noting challenges to do with timeliness and completeness of malaria death surveillance system. A pilot exercise was introduced in Manicaland province in 2022. The electronic form is a replica of the paper-based form. It is integrated in the web-based District Health Information System (DHIS2).
Manicaland had recorded the highest number of malaria deaths in 2020 and 2021. Health Information Officers (HIOs) and one nurse from each of the 25 hospitals in Manicaland were trained by NMCP. During the training, deaths from 2020 to 2022 were captured electronically and they were supposed to continue capturing deaths which occurred thereafter.
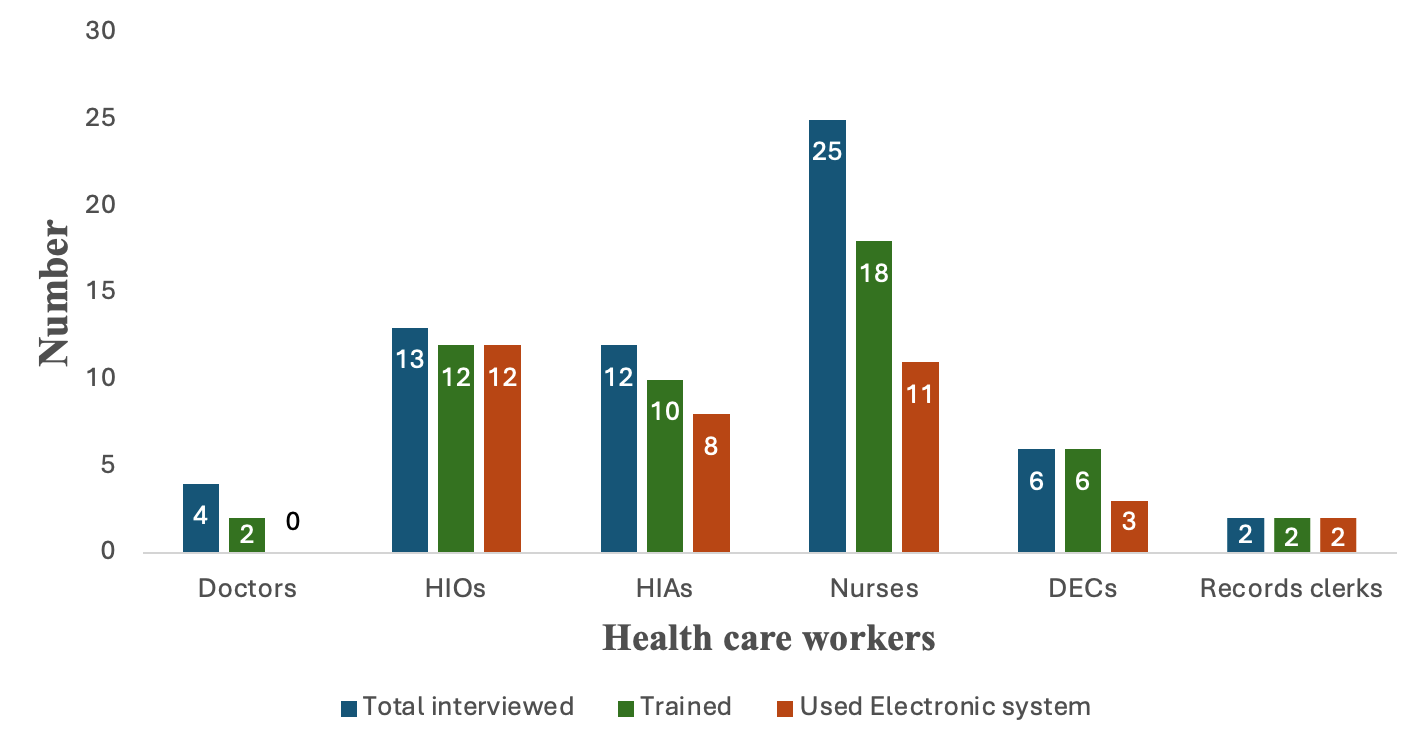
In this pilot electronic malaria death notification surveillance system, completion of the paper forms is done within 7 days by the nurses or doctors who then submit the forms to the HIOs who are stationed at the hospitals for electronic capturing. Districts make use of whatever means that are appropriate for them (hand submission or WhatsApp), to ensure that they meet the timeline. There is however no stipulated timeline for submission of the electronic form. Once the form is uploaded, it can be viewed by decision-makers at all levels in real-time. Each level analyzes data and takes appropriate action before the data is forwarded to the next level.[3]
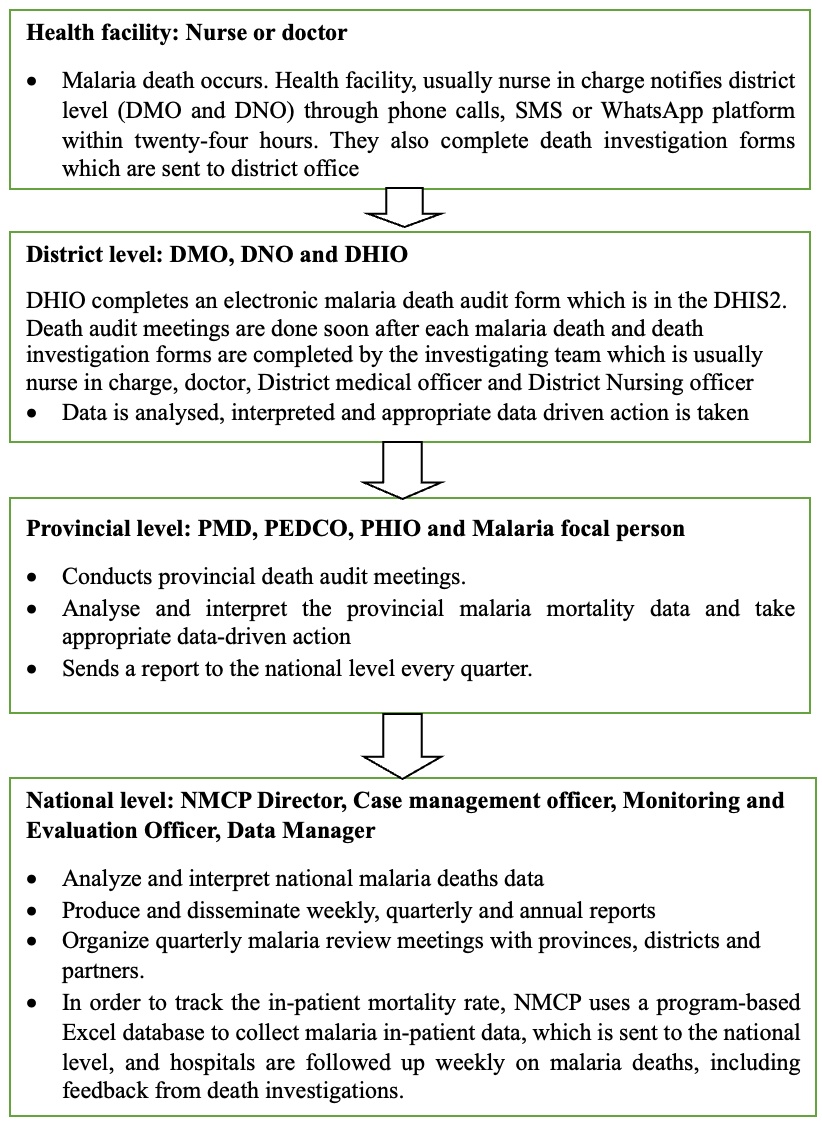
Death audit meetings are held at the district and provincial levels. In these meetings challenges are identified and reference is made to malaria case management Standard Operating Procedures.[4] Recommendations are made in order to improve severe malaria case management, reduce mortality and improve the surveillance system. This study sought to evaluate the electronic malaria death notification system in Manicaland province.[5] The flow of the electronic malaria death notification system is shown in Figure 1.
Methods
Study design
A descriptive cross-sectional study was conducted to evaluate attributes of the electronic malaria death notification surveillance system piloted in Manicaland province using the updated CDC guidelines for evaluating a public health surveillance system. [6]
The study was conducted at 11 hospitals from seven districts in Manicaland Province. That is, one provincial hospital, five district hospitals and five mission hospitals.
Study population
The study population comprised of nurses, doctors, Health Information Officers (HIOs) and Health Information Assistants (HIAs), Data Entry Clerks (DECs) and records clerks from hospitals in Manicaland. Key informants were the Data Manager, Monitoring and Evaluation Officer (M&E) for the National Malaria Control Programme (NMCP), Provincial Health Information Officer (PHIO), District Medical Officers (DMOs), and partners (Zimbabwe Assistance Programme in Malaria 11 (ZAPIM 11) and Clinton Health Access Initiative (CHAI).
Sample size calculation
The sample size was calculated using Dobson’s formula for the calculation of sample size for single proportions.
$$n = \frac{z^2 \times p(1 – p)}{d^2}$$
where:
n = sample size
d = margin of error (5%)
p = proportion.
The sample size was calculated based on a study by, Muchena et. al (2018), assuming that the timeliness of submission of malaria forms was at 28% [7]
z = confidence level at 95% (standard value 1.96), we calculated a minimum sample size (n) of 56 healthcare workers (HCW), plus a 10% attrition rate, which equals 62.
Sampling procedure
Eleven hospitals that had utilized the electronic malaria death notification system were included in the study, that is, one provincial hospital, five district hospitals and five mission hospitals. Sampling proportionate to size was used to determine the number of healthcare workers (HCWs) required from each hospital. The total study sample of 62 HCWs was allocated among the 11 hospitals such that each hospital’s allocated sample size was proportional to its number of health workers, using this formula
\[
\text{Hospital Sample size} =
\left(
\frac{\text{Number of HCWs at that hospital}}
{\text{Total number of HCWs at all 11 hospitals}}
\right)
\times \text{Estimated sample size of } 62 \text{ HCWs}
\]
Key informants were selected based on their expertise in using electronic malaria death notification system. Among them, the Data manager, M&E officer and partners who were involved in the development of both the paper-based and electronic forms.
Data collection and analysis
Data were collected using a pre-tested interviewer-administered questionnaire from 31 October 2023 to 12 November 2023. We reviewed the number of deaths reported in DHIS2 in Manicaland by health facility from 2020 to 2023. Interviewer-administered questionnaires were administered to HCWs to collect information on the reasons for failing to submit malaria death investigation forms, knowledge of the malaria death notification surveillance system among HCWs and attributes of the surveillance system. Key informant interview guides were used to get in-depth information. The questions were structured, semi-structured and open-ended. The interviews were done in person and data was recorded using the note-taking method. The average duration of each interview was 15 minutes. A checklist was used to assess for availability of resources for electronic malaria death investigation at the health facility. Minute books were reviewed to see if they held meetings to discuss about malaria deaths and assess the usefulness of the surveillance system.
Data analysis
Data analysis was done using Epi Info version 7.2.5. We generated frequencies, means, and proportions. A Likert scale was used to classify the knowledge of healthcare workers. Study participants were asked 10 questions, and each correct answer was awarded a single point. A score of 0-2 was poor, 3-5 was fair, 6-8 was good, and 9-10 was excellent. Qualitative data was analysed manually by identification, examination, and interpretation of patterns and themes to help answer the research question. Thematic analysis was conducted using inductive and deductive coding for key informant interviews. Transcripts were analysed manually, yielding 25 codes and 5 themes.
Ethical considerations
Permission to conduct the study was obtained from the Health Studies Office (HSO), the Provincial Medical Director (PMD) for Manicaland province, and the District Medical Officer (DMO) of all seven districts in Manicaland province. No ethical clearance was sought from an institutional review board because this activity was considered to be part of routine surveillance.
The researcher conducted the study ethically where the principles of confidentiality, informed consent, anonymity, and harm to participants were addressed. Participant names were not captured during data collection. Informants were fully informed about the evaluation and signed a consent form before responding to interview questions.
Results
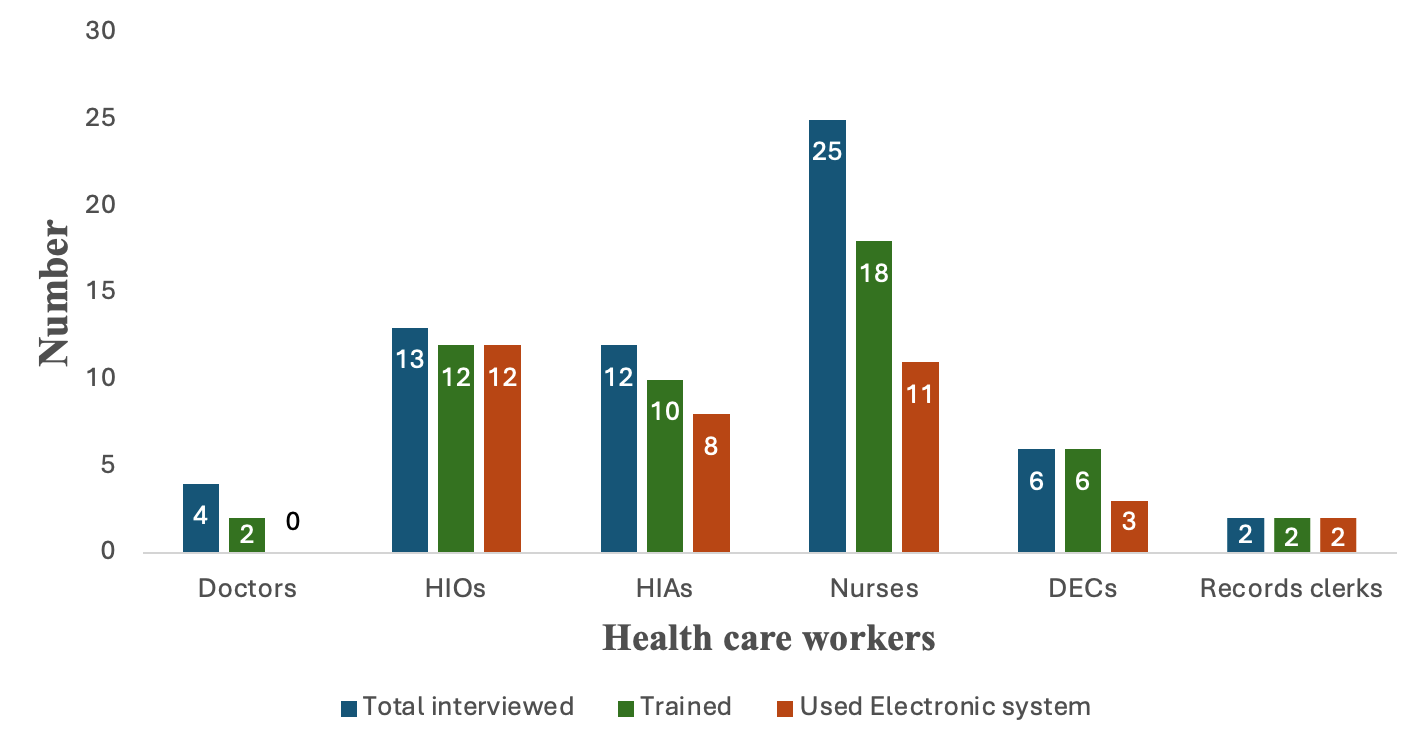
We interviewed 62 HCWs comprising four doctors (6.5%), 13 HIOs (20.9 %), 12 HIAs (19.4 %), 25 nurses (40.3 %), 6 Data Entry Clerks (DECS) (9.7%) and two records clerks (3.2 %). Most participants (58%) were female. Their median age was 31 years (IQR: 25-39). The median years in service was 9 (Q1=3; Q3=16).
As shown in Figure 2, out of the 62 participants, 18 (72%) nurses were trained to use the electronic system, but 7 (28%) of them had not used the system. While both records clerks were trained and used the system, all six data entry clerks were trained, but only three of them used the system. On the other hand, 12 of the 13 HIOs were trained and used the system, and 10 of the 12 HIAs were trained, but only eight used the system. Two out of four doctors were trained, but none had used the electronic system, Figure 2.
The training was conducted in August 2022. HIOs, HIAs, and nurses who were trained by NMCP had excellent knowledge levels. The knowledge level of the participants was varied, ranging from excellent to poor. Notably, all the 13 HIOs had excellent or good knowledge, while all four doctors had poor knowledge (Table 1).
Reasons for poor performance of the electronic malaria death surveillance system
Human resources: Fifty per cent of the 62 participants mentioned delays in the submission of paper-based forms due to delays by doctors to complete their section on the form. Five per cent mentioned a lack of knowledge and staff shortage.
Two facilities did not have a malaria focal person, and 20% said that malaria death notification was not being prioritised. Fifteen per cent stated a lack of communication between departments.
Equipment/material related: Ten per cent of study participants mentioned that sometimes paper-based forms will not be available due to a shortage of stationery and printing equipment. Poor network connectivity was highlighted at three health facilities. Two out of 13 HIOs (15%) did not have laptops. Airtime was said to be sometimes not available by 68% of study participants.
Usefulness of the system
The introduction of the electronic malaria death investigation form has led to improved surveillance and response to malaria-related deaths in real-time. The electronic data collection tools have enabled the district to have automated data analysis and visualisation capabilities, resulting in rapid detection of trends and patterns, facilitating prompt investigations and targeted interventions. Evidence of such was the early identification of 2022 and 2023 malaria outbreaks and redistribution of malaria commodities to highly burdened facilities..
Flexibility
The electronic system was integrated with the already existing DHIS2 platform. However, 40% of the 62 participants said the electronic form did not accommodate data from the private sector. Also, there was no room to record the hospital ward from which the death is reported so as to analyse trends at that level.
Simplicity
Eighty per cent of the 62 participants mentioned that the system was easy to use and to edit. To complete the electronic form, 60% of participants required between 5 to 10 minutes, 30% required 10 to 15 minutes and 10% needed more than 15minutes.
Acceptability
HIOs and HIAs knew that it was their duty to complete the electronic form and 10% of nurses and DECs said that it was the duty of either the nurses or doctors. All participants wanted the electronic malaria death notification surveillance system to continue, stating that it is necessary, convenient, time-saving, reduces bulky paper in offices and allows data dissemination in real-time.
Representativeness
The surveillance system excluded private health facilities. This was mentioned by 40% of the 62 participants. However,50% of participants said that exclusion of the private sector did not affect the system’s representativeness because the private facilities in the province comprise of clinics and surgeries, and they refer severe patients to the hospitals. However, this information could not be verified.
Stability
The DHIS2 had an uptime of more than 80% in the previous quarter, and it had a less than 1% error rate in data transmission. It also has daily backups and quick data recovery processes to prevent data loss. There was evidence of high user adoption and retention rates of over 90% indicating reliability and usability of the system.
Timeliness
As shown in Table 2, 50% of study participants notified malaria deaths electronically within a week, 34% within a fortnight and 10% required more than 2 weeks. Six per cent were notified within 24 hours. There were, however, no guidelines stipulating expected timelines.
Completeness
Fifty forms were reviewed. On average, five forms per health facility. The section on demographics had the highest number of fields with missing data, especially the phone number and occupation on both the paper-based and electronic forms. Reasons given for missing phone numbers were that some patients either did not know their numbers or they did not have a phone. Some forms were said to be submitted without the doctor’s signature or with missing dates and they would be returned to the doctor resulting in further delays regarding electronic capturing.
The electronic system did not allow for zero reporting. If a health facility did not report a death, the next level will assume that they had no deaths during that reporting period.
Sensitivity
Out of the 11 hospitals, 5 did not provide the paper-based forms for the interviewers to review, but other source documents (hospital admission and discharge registers and mortality registers) were also used to verify the proportion of malaria-related deaths and the accuracy of captured details. Notably, all malaria-related deaths had been captured electronically.
Estimated running cost
The estimated annual costs of running the electronic malaria death surveillance system at the 11 hospitals in Manicaland were divided into recurrent costs (USD 3,000) and once-off costs (USD 368). One-off costs included training costs, wireless internet router and installation fees, while recurrent costs included Wi-Fi subscriptions.
Findings from key informant interviews
Findings from key informant interviews yielded valuable insights into the electronic malaria death surveillance system. They highlighted that the system was simple to use but they also mentioned that there were challenges to do with poor network connectivity which resulted in delayed submission. “The form is easy to use even for those with basic computer literacy”.
Some key informants highlighted the need to train healthcare workers. “Training improves completeness and timeliness” [Key Informant 3]. They also mentioned that the representativeness of the system was affected by its exclusion of the private sector. “The number of malaria deaths being missed was said to be unknown. “There is a need to review our policies so that they address this underreporting”. The major reason given by key informants for the poor performance of the electronic malaria death surveillance system was poor prioritization by managers. “If any system is to run well, there is need to ensure that district accounting officers are sensitized and trained” [Key Informant 4]. “Most health facilities have Wi-Fi and solar systems in place as backup plan in case of power outages” [Key Informant 5]. The costs of running the electronic system were also said to be affordable and sustainable.
Discussion
Knowledge level
Most HIOs and nurses had good knowledge. This could be attributed to the targeted training that was done by NMCP in August 2022. The good knowledge of HIAs and DECs could be attributed to the on job training conducted by the trained cadres. Wangdi et al. (2020) in his study in Solomon Islands mention the need for training since it addresses knowledge gaps.[8]. This was seen to affect timeliness, sensitivity and completeness. Lack of knowledge was seen to result in HCWs not collecting or not entering data correctly leading to incomplete or inaccurate data. In some cases, the few individuals who had the knowledge were left to do the reporting, resulting in work overload which affects data quality. English et al (2018) highlights the importance of HCW knowledge in enhancing the quality of mortality data. [9]
Usefulness
The surveillance system was useful since the HCWs use the data for planning awareness campaigns for the community, identification of at-risk groups, monitoring and evaluation, epidemic detection and assessing achievements. The World Health Organization (WHO) Malaria Elimination Framework 2021-2025 outlines that a useful surveillance system should support timely decision-making, inform policy, planning, resource allocation, and accurately describe malaria transmission patterns. [10].
Timeliness
There was no stipulated timeline for the HIOs to capture the forms electronically. Half of the participants notified deaths within 7 days, and more than a quarter notified within 2 weeks. Delay in malaria death notification hinders timely investigation and intervention. WHO (2016) highlights the need for a robust real-time malaria death notification system [11]. These findings are unlike those by English et al. (2018) where 80% submitted electronic reports within 2 days. [9] The lack of guidelines was seen to be the major gap which needs to be addressed by the NMCP. Chizema-Kawesha et al. (2016) stresses the need for standardized malaria mortality notification. [12] Quan (2014) in a study done in South Africa found that timeliness of notifications improved by more than 50% when reporting forms were digitalised. [13] Timeliness of reporting was found to improve when individuals were assigned to perform specific tasks, which ensured accountability. [14]
Flexibility
The electronic system was flexible since it is integrated with the DHIS2 platform, which the country was already using to monitor other public health events. This agrees with the findings of Wangdi et al. (2020) in a study done in Solomon Islands, where the electronic system was found to be flexible as it was integrated with other health surveillance systems [8]. Integration of this form in the DHIS2 implies that reporting can be done in real-time, data analysis is easier and other data elements like comorbidities and time taken before presentation at the health facility could be easily assessed. Quan (2014) mentions that a flexible system allows HCWs to enter data when there was poor network connectivity and allowed them to synchronize the data into the DHIS2 when they reached areas of good network connectivity. [13] However, the flexibility is compromised since the current system does not accommodate capturing data from private sector facilities and the name of the hospital ward where the death occurred and yet it is easy to add, remove or update the variables in DHIS2.
Simplicity
The surveillance system was simple. The majority of study participants (60%) took on average 5 to 10 minutes to complete the three-page form, implying that the form was simple to complete. The others required more time to complete the form because they would not sit and complete the form at once without pausing to attend to other duties. Ten per cent had a slow typing speed. This is consistent with findings of a similar study in South Africa by Mabona et al. (2024) where over half (64%, 9/14) of the respondents agreed that they found it simple to share, transfer, enter, edit, and store data on DHIS2. [15]
Sensitivity
The fact that all malaria-related deaths were captured electronically suggests that the electronic system is comprehensive and effective in recording malaria deaths. This reiterates the reliability of electronic reporting but however, emphasises the need for regular monitoring and evaluation exercises.
Completeness
Approximately only half of the reviewed forms were complete and one of the reasons given was that doctors delayed completing their section. In a study in 3 provinces of Zimbabwe by Chung et al. (2020), completeness, among other attributes, improved when the provinces invested in improving teamwork among HCWs. [14]
Githinji et al. (2017) mentioned that the completeness of data was comparable between the electronic system and the paper-based system. The finding was however inconsistent with this study which found that the two systems were the same in terms of low data completeness. This was because the electronic system was dependent on the paper-based system since the two systems were running concurrently. The electronic form could not be completed without a paper form to refer to. Missing data was mostly on the demographics section, specifically contact details. This is unlike findings of Mabona et al. (2024) where in South Africa, less than 1% of forms had uncompleted fields under demographics. They however found that only 41.6% of fields under symptoms and 63.5% of fields under travel history had information, the rest of the fields were blank or labelled “unknown” This is unlike in the study in Ghana where missing data was mostly coordinates. [15,16]
Representativeness
Exclusion of the private sector data can create biased surveillance as only public sector data is considered, potentially skewing trends and patterns. Similarly, in a study by Muchena et al. (2018), the private sector was excluded. [7] Githinji et al. (2017) explicitly mention that they excluded data from the private sector due to inconsistent reporting and a lack of standardised reporting since the private sector uses different reporting tools and channels. [16] Private health facilities may serve certain populations or geographical areas, and excluding them may lead to inadequate representation of these groups in surveillance data. According to Mabona et al. (2024) in a study in South Africa, the private sector was included but their data was incomplete and resulting in missed opportunities for early detection, targeted interventions and effective disease control. [15] This implies reduced collaboration between the public and private sectors, hindering effective disease control.
Limitations
The paper-based system was running concurrently with the electronic system and was the data source of the latter. This directly affected the performance of the electronic system. Also, the study was done among hospitals only since clinics were not included in the pilot. If this system is introduced to clinics, the performance could be different.
Conclusion
The electronic malaria death surveillance system was simple, flexible, acceptable and useful. It was poor on timeliness due to poor knowledge of reporting deadlines and a delay in submission of paper-based forms. Its sensitivity was compromised because it excluded deaths at private health facilities. We recommend rolling out the electronic system to other provinces once the identified gaps are addressed and the guidelines are developed (Table 3).
What is already known about the topic
- Electronic reporting improves timeliness, completeness and sensitivity.
- Achieving the optimum of these attributes is attributed to a lack of resources
What this study adds
- Identification of gaps which should be addressed before rolling out the programme to other provinces.
- Insights from users of both the electronic and paper-based system.
Authors´ contributions
Delight Mhungira and Patience Dhliwayo did the conception and design of the study, data collection, analysis and interpretation, and manuscript writing. Addmore Chadambuka, Gerald Shambira, Notion Gombe, Tsitsi Juru, Gibson Mandozana, and Mufuta Tshimanga did the conception, design, data analysis, interpretation, critical revision, and final approval of the study. All authors read and agreed to the final manuscript.
| Cadre of health worker | Excellent | Good | Fair | Poor | Total |
|---|---|---|---|---|---|
| Doctors | 0 | 0 | 0 | 4 | 4 |
| Nurses | 4 | 10 | 11 | 0 | 25 |
| HIOs | 7 | 6 | 0 | 0 | 13 |
| HIAs | 1 | 9 | 2 | 0 | 12 |
| DECs | 1 | 4 | 1 | 0 | 6 |
| Records clerks | 0 | 1 | 1 | 0 | 2 |
| Time taken to submit the electronic form | Frequency (%) |
|---|---|
| 24 hours | 4 (6) |
| Within 7 days | 31 (50) |
| Within 2 weeks | 21 (34) |
| More than 2 weeks | 6 (10) |
| Key Finding | Recommendation | Responsible person | Timeline |
|---|---|---|---|
| Delayed submission of paper-based forms due to delay by doctors to complete their section on the form. | • To have guidelines which clearly stipulate the timelines • Doctors or nurses who attended the deceased should complete the form as a team as soon as the death occurs • Phase out the paper-based forms in Manicaland | NMCP District Medical Officer (DMO) and District Nursing Officer (DNO) NMCP | 01-06-24 Immediately 01-06-24 |
| Fifteen out of 50 (30%) of the reviewed forms had incompletely filled forms. | • Put required fields on the form | NMCP Data manager | 09-02-24 |
| Poor knowledge of the electronic system was mainly among doctors and nurses. | • Malaria death notification trainings should include doctors and nurses • Malaria electronic death notification should be assessed during quarterly support and supervision | Provincial Medical Director (PMD) | 15-02-24 Immediately |
| Fields on the electronic form are not in sequence and the field for age does not accommodate age less than 1. | Revise the electronic form | NMCP- Data manager | 05-02-24 |
| Inadequate airtime | Include airtime for Health Information Officers in the hospital budgets | DMO | 15-02-24 |
References
- RBM Partnership to End Malaria. Strengthening of the activities of National Malaria Elimination Programmes in the cross-border areas of South-East Asia countries to accelerate malaria elimination [Internet]. Copenhagen (Denmark): RBM Partnership to End Malaria; 2022 Mar 18 [cited 2025 Nov 7]. [about 2 screens]. Available from: https://endmalaria.org/opportunities/strengthening-activities-national-malaria-elimination-programmes-cross-border-areas
- Ministry of Health and Child Care (Zimbabwe). 2022 Malaria Report. Harare, Zimbabwe: Ministry of Health and Child Care; 2023 [cited 2025 Nov 10] 13 p.
- Mbunge E, Millham R, Sibiya N, Takavarasha S. Is malaria elimination a distant dream? Reconsidering malaria elimination strategies in Zimbabwe. Public Health in Practice [Internet]. 2021 Jul 29 [cited 2025 Nov 7];2:100168. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666535221000938 https://doi.org/10.1016/j.puhip.2021.100168
- Sande S, Zimba M, Chinwada P, Masendu HT, Mberikunshe J, Makuwaza A. A review of new challenges and prospects for malaria elimination in Mutare and Mutasa Districts, Zimbabwe. Malar J [Internet]. 2016 Jul 3 [cited 2025 Nov 7];15(1):360. Available from: http://malariajournal.biomedcentral.com/articles/10.1186/s12936-016-1415-2 https://doi.org/10.1186/s12936-016-1415-2
- Mutsigiri F, Mafaune PT, Mungati M, Shambira G, Bangure D, Juru T, Gombe NT, Tshimanga M. Malaria morbidity and mortality trends in Manicaland province, Zimbabwe, 2005-2014. Pan Afr Med J [Internet]. 2017 May 11 [cited 2025 Nov 7];27. Available from: http://www.panafrican-med-journal.com/content/article/27/30/full/
- Centers for Disease Control and Prevention. Updated guidelines for evaluating public health surveillance systems: recommendations from the guidelines working group. MMWR [Internet]. 2001 Jul 27 [cited 2025 Nov 7];50(No. RR-13). Available from: https://www.cdc.gov/mmwr/pdf/rr/rr5013.pdf
- Muchena G, Dube B, Chikodzore R, Pasipamire J, Murugasampillay S, Mberikunashe J. A review of progress towards sub-national malaria elimination in Matabeleland South Province, Zimbabwe (2011–2015): a qualitative study. Malar J [Internet]. 2018 Apr 3 [cited 2025 Nov 7];17(1):146. Available from: https://malariajournal.biomedcentral.com/articles/10.1186/s12936-018-2299-0 https://doi.org/10.1186/s12936-018-2299-0
- Wangdi K, Sarma H, Leaburi J, McBryde E, Clements ACA. Evaluation of the malaria reporting system supported by the district health information system 2 in solomon islands. Malar J [Internet]. 2020 Oct 17 [cited 2025 Nov 7];19(1):372. Available from: https://malariajournal.biomedcentral.com/articles/10.1186/s12936-020-03442-y https://doi.org/10.1186/s12936-020-03442-y
- English M, Mwaniki P, Julius T, Chepkirui M, Gathara D, Ouma PO, Cherutich P, Okiro EA, Snow RW. Hospital Mortality – a neglected but rich source of information supporting the transition to higher quality health systems in low- and middle-income countries. BMC Med [Internet]. 2018 Dec [cited 2025 Nov 7];16(1):32. Available from: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1024-8 https://doi.org/10.1186/s12916-018-1024-8
- Pan American Health Organization / World Health Organization (Regional Office for the Americas). Plan of Action for Malaria Elimination 2021-2025 [Internet]. Washington (D.C): World Health Organization (Regional Office for the Americas); 2022 [cited 2025 Nov 7]. 27 p. Available from: https://iris.paho.org/handle/10665.2/56616 Download PAHOCDEVT/220005_eng.pdf
- World Health Organization. Eliminating malaria in the Greater Mekong Subregion: United to end a deadly disease [Internet]. Geneva (Switzerland): World Health Organization; 2016 Nov 10 [cited 2025 Nov 7]. 24 p. Available from: https://www.who.int/publications/i/item/WHO-HTM-GMP-2016.12 Download WHO-HTM-GMP-2016.12-eng.pdf
- Chizema-Kawesha E, Miller JM, Steketee RW, Mukonka VM, Mukuka C, Mohamed AD, Miti SK, Campbell CC. Scaling up malaria control in Zambia: progress and impact 2005–2008. The American Society of Tropical Medicine and Hygiene [Internet]. 2010 Sep [cited 2025 Nov 7];83(3):480–8. Available from: https://www.ajtmh.org/view/journals/tpmd/83/3/article-p480.xml https://doi.org/10.4269/ajtmh.2010.10-0035
- Quan V, Hulth A, Kok G, Blumberg L. Timelier notification and action with mobile phones–towards malaria elimination in South Africa. Malar J [Internet]. 2014 Apr 21 [cited 2025 Nov 7];13(1):151. Available from: https://malariajournal.biomedcentral.com/articles/10.1186/1475-2875-13-151 https://doi.org/10.1186/1475-2875-13-151
- Chung AM, Case P, Gosling J, Gosling R, Madinga M, Chikodzore R, Hove M, Viljoen G, Chitapi P, Gumbi M, Mnguni P, Murungu J, Dube B, Dhliwayo P, Mberikunashe J. Scaling up malaria elimination management and leadership: a pilot in three provinces in Zimbabwe, 2016–2018. Malar J [Internet]. 2020 May 20 [cited 2025 Nov 7];19(1):185. Available from: https://malariajournal.biomedcentral.com/articles/10.1186/s12936-020-03255-z https://doi.org/10.1186/s12936-020-03255-z
- Mabona M, Zwane T, Raman J, Kuonza L, Mhlongo B, Phafane P. Evaluation of the malaria case surveillance system in KwaZulu-Natal Province, South Africa, 2022: a focus on DHIS2. Malar J [Internet]. 2024 Feb 14 [cited 2025 Nov 7];23(1):47. Available from: https://malariajournal.biomedcentral.com/articles/10.1186/s12936-024-04873-7 https://doi.org/10.1186/s12936-024-04873-7
- Githinji S, Oyando R, Malinga J, Ejersa W, Soti D, Rono J, Snow RW, Buff AM, Noor AM. Completeness of malaria indicator data reporting via the District Health Information Software 2 in Kenya, 2011–2015. Malar J [Internet]. 2017 Aug 17 [cited 2025 Nov 7];16(1):344. Available from: http://malariajournal.biomedcentral.com/articles/10.1186/s12936-017-1973-y https://doi.org/10.1186/s12936-017-1973-y
