Research | Open Access | Volume 8 (4): Article 91 | Published: 12 Nov 2025
Factors associated with the COVID-19 vaccine hesitancy in the Western North Region, Ghana
Menu, Tables and Figures
On Pubmed
Navigate this article
Tables
Table 1: Sociodemographic characteristics of the respondents, N=450
| Characteristics | Number (Percent) |
|---|---|
| Age (years) | |
| 15–24 | 149 (33.11) |
| 25–29 | 145 (32.22) |
| 30–44 | 73 (16.22) |
| 45+ | 83 (18.44) |
| Gender | |
| Female | 277 (61.6) |
| Male | 173 (38.4) |
| Education | |
| Primary | 66 (14.7) |
| JHS | 163 (36.2) |
| Secondary | 115 (25.5) |
| Tertiary | 36 (8.0) |
| None | 70 (15.6) |
| Employment status | |
| Government employed | 22 (4.9) |
| Self-employed | 239 (53.1) |
| Unemployed | 189 (42.0) |
| Marital status | |
| Married | 176 (39.1) |
| Single | 273 (60.7) |
| Won’t say | 1 (0.2) |
| Income status | |
| Above GHC 2000 | 11 (2.4) |
| GHC 1000–2000 | 34 (7.6) |
| GHC 500–1000 | 81 (18.0) |
| Less than GHC 500 | 146 (32.4) |
| Won’t say | 178 (39.6) |
| Area of residence | |
| Rural | 324 (72.0) |
| Urban | 126 (28.0) |
Table 1: Sociodemographic characteristics of the respondents, N=450
Table 2: Bivariate (Chi-Square test) analysis of sociodemographic factors associated with COVID-19 vaccine hesitancy
| Variables | Hesitant 271 (60.22%) | Non-Hesitant 179 (39.78%) | p-value |
|---|---|---|---|
| Age | |||
| 15–24 | 84 (31.0) | 65 (36.31) | 0.518 |
| 25–34 | 93 (34.3) | 52 (29.05) | |
| 35–44 | 42 (15.49) | 31 (17.32) | |
| 45+ | 52 (19.19) | 31 (17.32) | |
| Gender | |||
| Female | 161 (59.41) | 116 (64.80) | 0.250 |
| Male | 110 (40.59) | 63 (35.20) | |
| Education Status | |||
| Primary | 33 (12.18) | 22 (12.18) | 0.035 |
| JHS | 100 (36.90) | 63 (35.20) | |
| Secondary | 68 (25.09) | 47 (26.26) | |
| Tertiary | 18 (6.64) | 18 (10.06) | |
| None | 52 (19.19) | 18 (10.06) | |
| Employment | |||
| Government employed | 7 (2.58) | 15 (8.38) | <0.001 |
| Self-employed | 162 (59.78) | 77 (43.02) | |
| Unemployed | 101 (37.64) | 87 (48.42) | |
| Marital Status | |||
| Married | 114 (42.07) | 65 (36.3) | 0.222 |
| Single | 157 (57.93) | 114 (63.7) | |
| Place of Residence | |||
| Rural | 187 (69.00) | 137 (76.54) | |
| Urban | 84 (31.01) | 42 (23.46) | |
| Information on COVID-19 Vaccination | |||
| Yes | 264 (97.42) | 168 (93.85) | 0.059 |
| No | 7 (2.58) | 11 (6.15) | |
Table 2: Bivariate (Chi-Square test) analysis of sociodemographic factors associated with COVID-19 vaccine hesitancy
Table 3: Multivariate logistic regression analysis of sociodemographic factors associated with COVID-19 vaccine hesitancy
| Variables | aOR (95% CI) | P-value |
|---|---|---|
| Age (years) | ||
| 15–24 | Ref | |
| 25–34 | 0.886 (0.523 – 1.501) | 0.652 |
| 35–44 | 1.314 (0.666 – 2.592) | 0.430 |
| 45+ | 1.230 (0.634 – 2.386) | 0.540 |
| Gender | ||
| Female | Ref | |
| Male | 0.726 (0.477 – 1.104) | 0.134 |
| Educational level | ||
| None | Ref | |
| JHS | 1.956 (0.992 – 3.857) | 0.053 |
| Primary | 2.917 (1.369 – 6.216) | 0.006 |
| Secondary | 2.167 (1.042 – 4.503) | 0.038 |
| Tertiary | 1.994 (0.713 – 5.578) | 0.188 |
| Employment status | ||
| Unemployed | Ref | |
| Government employed | 2.338 (0.765 – 7.147) | 0.136 |
| Self-employed | 0.596 (0.384 – 0.926) | 0.021 |
| Marital status | ||
| Married | Ref | |
| Single | 1.151 (0.723 – 1.832) | 0.555 |
| Area of residence | ||
| Rural | Ref | |
| Urban | 0.635 (0.404 – 0.997) | 0.049 |
| Hearing information on the COVID-19 vaccine | ||
| No | Ref | |
| Yes | 0.447 (0.160 – 1.254) | 0.126 |
Table 3: Multivariate logistic regression analysis of sociodemographic factors associated with COVID-19 vaccine hesitancy
Figures


Keywords
- Vaccine, Hesitancy
- COVID-19
- Western North
- Ghana
Marion Okoh-Owusu1, Joshua Billy1,&, Kingsley Osei-Kwakye1, Osei Sakyi1, Patrick Avevor2, Therson Mintah1, Sally-Ann Ohene2, Francis Chisaka Kasolo2, Patrick Kuma-Aboagye3
1Regional Health Directorate, Ghana Health Service, Western North Region, Bodi, Ghana, 2World Health Organisation, Ghana Country Officer, Accra. Ghana, 3Ghana Health Service, Headquarters, Accra. Ghana
&Corresponding author: Joshua Billy, Regional Health Directorate, Ghana Health Service, Western North Region, Bodi, Ghana, Email: josebilly35@gmail.com ORCID: https://orcid.org/0009-0002-9250-8161
Received: 10 Dec 2024, Accepted: 10 Nov 2025, Published: 12 Nov 2025
Domain: COVID-19 Pandemic, Vaccinology
Keywords: Vaccine, Hesitancy, COVID-19, Western North, Ghana
©Marion Okoh-Owusu et al. Journal of Interventional Epidemiology and Public Health (ISSN: 2664-2824). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Marion Okoh-Owusu et al., Factors associated with the COVID-19 vaccine hesitancy in the Western North Region, Ghana. Journal of Interventional Epidemiology and Public Health. 2025;8(4):91. https://doi.org/10.37432/jieph-d-24-02027
Abstract
Introduction: Vaccines are one of the most effective tools developed for reducing the spread and mitigating the impact of outbreaks such as the COVID-19 pandemic. However, vaccination campaigns have been met with hesitancy, fear, and concerns about safety, coupled with anti-vaccine messages, which significantly compromise willingness to accept the vaccine. This study aimed to examine the factors associated with vaccine hesitancy in the Western North Region of Ghana, which had been recording low COVID-19 vaccination coverage after several rounds of vaccination campaigns
Methods: A cross-sectional survey of 450 unvaccinated or partially vaccinated individuals was conducted in the Western North Region of Ghana using a multi-stage cluster sampling design. Data were collected with a validated questionnaire adapted from the WHO SAGE Vaccine Hesitancy scale. Descriptive statistics, bivariate and multivariate logistic regression were employed to identify factors associated with COVID-19 vaccine hesitancy. Ethical approval was obtained from the Ghana Health Service Ethics Review Committee.
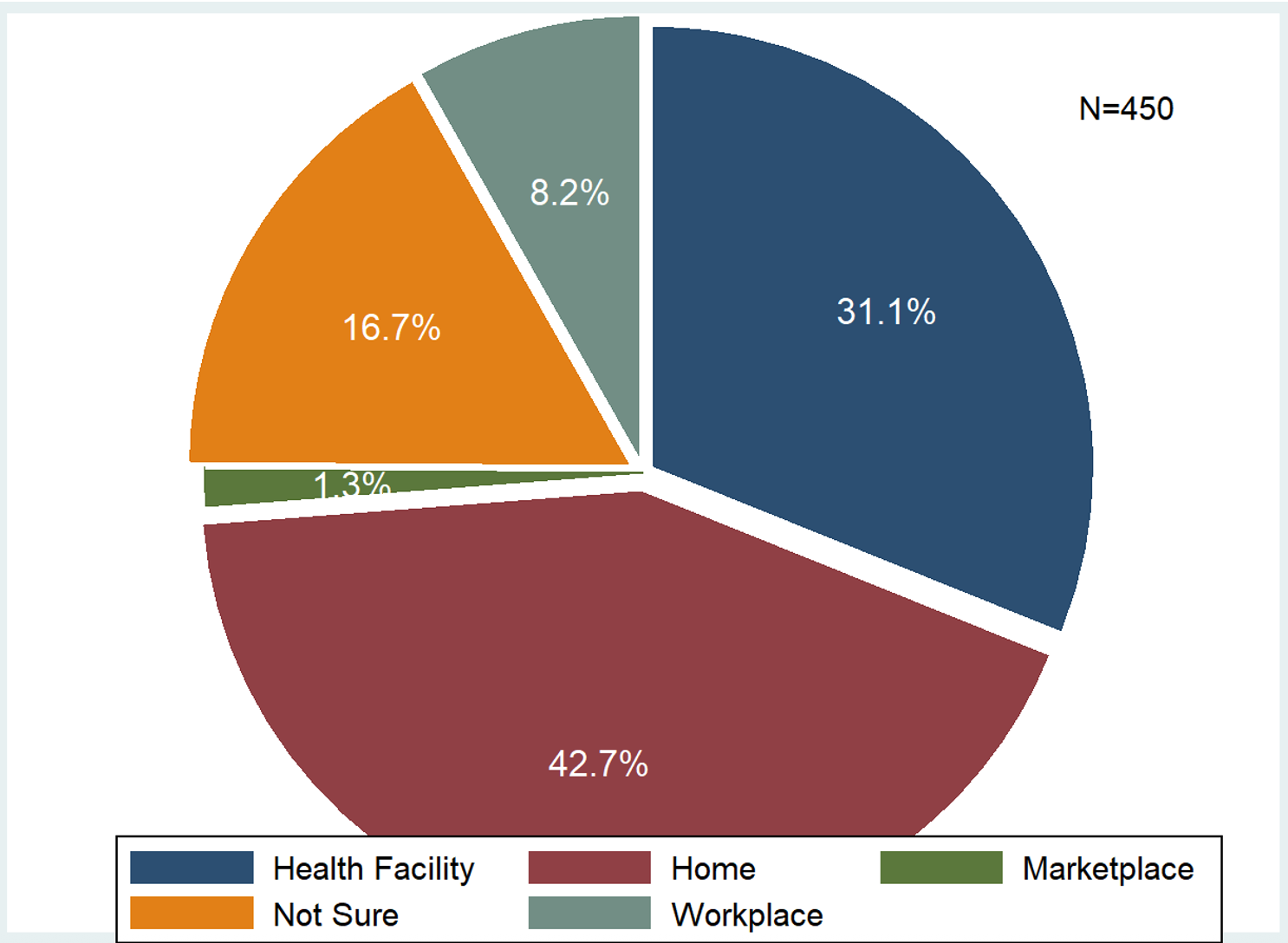
Results: Out of the 450 participants in the Western North Region of Ghana, 60.22% demonstrated COVID-19 vaccine hesitancy. The study population was predominantly female (61.6%), self-employed (53.1%), and rural-dwelling (72.0%). Bivariate analysis revealed significant associations between hesitancy and both employment status (p<0.001) and educational attainment (p=0.035). The multivariate model identified three independent predictors: compared to no formal education, primary (aOR=2.92; 95% CI:1.37-6.22) and secondary education (aOR=2.17; 95% CI:1.04-4.50) significantly increased odds of hesitancy. Conversely, self-employment reduced odds by 40% versus unemployment (aOR=0.60; 95% CI:0.38-0.93), and urban residence reduced odds by 36% versus rural areas (aOR=0.64; 95% CI:0.40-1.00). Primary concerns driving hesitancy were side effects (33.54%) and concerns on fertility (31.06%). Despite high information exposure (96.2%), mainly through television (67.90%) and radio (20.32%), this did not translate to high acceptance. Notably, 42.7% preferred home-based vaccination, suggesting accessibility remains a crucial barrier.
Conclusion: This study reveals that COVID-19 vaccine hesitancy in the Western North Region of Ghana is influenced by concerns regarding side effects, fertility, and sociodemographic factors such as education and employment. Effective communication and community-based strategies are essential to address misinformation and improve vaccine confidence and acceptance.
Introduction
The COVID-19 outbreak began in December 2019 in Wuhan, China, when several people were diagnosed with pneumonia, the cause of which was unknown. The causative agent for the disease (Coronavirus disease 2019 or COVID-19) was later identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The COVID-19 pandemic has taken a tremendous toll on the social and economic progress of several nations worldwide [1]. To limit the spread of COVID-19 and its impact, it is necessary to protect the population by achieving herd immunity. A safer way to do this, as recommended by the WHO, is through vaccination [2].
Vaccines constitute one of the most successful public health measures against pandemics and viral outbreaks [3,4]. According to Z. Al-Mansour et al. (2017), millions of lives have been saved because of the substantial contributions of vaccines to the elimination of global diseases [5]. Despite the benefits of vaccines, some people do not accept them, or it takes them some time to be convinced to be vaccinated. This behaviour, which is known as vaccine hesitancy, has been defined by the WHO as “delay in acceptance or refusal of vaccination despite availability of vaccination services. Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence.” [6].
Complacency, convenience, and confidence form the “3Cs” model, according to the WHO EURO Vaccine Communications Working Group in 2011 [7]. Complacency refers to the perceived low risk of the disease for which the vaccine is being given and the need for vaccination; convenience is about access and availability, while confidence indicates trust in the safety and effectiveness of the vaccine as well as the competence of the health system delivering the vaccine [6,8].
Hesitancy against vaccines occurs in both developed and lower-middle-income countries [8,9]. It has also been found to fluctuate globally depending on the time of assessment. Several factors influence or determine vaccine hesitancy, among which are religion, education, gender, apprehensions relating to side effects of the vaccines, trust in the health system, among others [8,9].
A review of the literature shows varying results regarding the role of socio-demographic factors on vaccine hesitancy. For example, Troiano and Nardi found different results regarding the influence of socioeconomic variables such as age, education, and income [9]. A study by Arce et al. also revealed mixed evidence on the effect of gender, education, and age in lower-middle-income countries (LMICs) on vaccine hesitancy [8]. The influence of ethnicity has also been found to be different in the literature, while Troiano and Nardi concluded that blacks or Africans were more vaccine-hesitant, contrary evidence was presented by Arce et al [8,9].
Low perceptions of the risk of being infected with COVID-19 and low mortality from the disease in Africa as compared to other developed countries, are also contributory factors to vaccine hesitancy on the continent [10]. The level of knowledge about COVID-19 vaccines (which can be linked to sources of information such as government, traditional and social media, and frequency of contact with these sources) also influences the rate of their uptake. Mistrust towards a government can negatively affect the reception of health information and education on COVID-19 disease, and requests by government officials to the citizenry to get vaccinated [6,11,12].
As of March 2022, approximately 40% of the global population had not received a single dose of any of the COVID-19 vaccines [13]. Within the same period in Ghana, only 14.4% had been fully vaccinated [14]. The Western North region has been recording low COVID-19 vaccine coverage after several rounds of vaccination campaigns – as at November 2022, 337,213 (48.3%) of the eligible population had received only the first dose of the COVID-19 vaccine and only 277,698 (39.8%) were fully vaccinated out of the eligible population of 697,564 [15].
Though there have been some studies that have looked at vaccine hesitancy in Ghana [16,17]. To the best of our knowledge, no studies have examined vaccine hesitancy in any particular region in the country. We conducted this study to examine the factors that contribute to COVID-19 vaccine hesitancy in the Western North region of Ghana to inform policy and strategies for improving vaccine uptake.
Methods
Study design and population
A cross-sectional survey was conducted in all nine (9) districts in the Western North Region of Ghana (Sefwi Wiawso, Bibiani-Anhwiaso-Bekwai, Aowin, Bia-West, Juaboso, Akontombra, Bia-East, Bodi and Suaman). The study was designed to assess factors influencing COVID-19 vaccine hesitancy, guided by a systematic review of existing literature. Key factors that were identified included trust in healthcare systems, exposure to misinformation, and sociodemographic barriers, which informed the development of the research instrument.
The survey instrument was adapted from the WHO SAGE Vaccine Hesitancy Scale [18–20], selected for its validated assessment of vaccine-related attitudes and behaviours. To ensure contextual relevance, modifications were made to question wording, response options, and language to align with local dialects, literacy levels, and cultural beliefs. Additional constructs from the USAID COVID-19 Vaccine Hesitancy Report [21–24] were incorporated to capture region-specific factors such as religious influences, healthcare accessibility, and trust in local providers.
The adapted questionnaire was pretested in two districts (Asawinso in Sefwi Wiawso and Bonsu Nkwanta in Juaboso) with a sample of 20 participants to evaluate clarity, comprehension, and reliability. Ambiguous questions were refined, and internal consistency was confirmed. Final adjustments were made to optimise question structure before full-scale deployment. The finalised questionnaire was administered to respondents by trained research assistants in each of the nine (9) districts in October 2022.
Study settings and participants
The study was conducted in the Western North Region of Ghana. Western North is one of the six (6) regions created in 2019. The region shares borders with Côte d’Ivoire to the West, the Central region to the Southeast, and the Ashanti, Ahafo and Bono regions to the North [25,26]. Different groups of people periodically move into the area to work on cocoa farms. The population of the Western North Region is approximately 898,540 [27].
The Western North Region of Ghana has a tropical rainforest climate, characterised by temperatures between 25°C and 30°C and an annual rainfall of 1,200–1,780 mm, which supports extensive agriculture, primarily cocoa farming [28]. The Region’s fertile land attracts diverse ethnic groups, which is a key sociodemographic variable included in our analysis to assess its influence on vaccine attitudes and helps in the generalisability of this research. The economy is primarily agrarian, reliant on cocoa and timber, which influences seasonal mobility and access to health services. Critically, the region faces significant healthcare access challenges, including a doctor-to-patient ratio of 1:25,000 and a nurse-to-population ratio of 1:1,750 [29]. These contextual factors of ethnicity, occupation, and healthcare access were operationalised as independent variables in our survey to explicitly test their hypothesised impact on vaccine uptake, a relationship highlighted as critical in prior literature [30]. Administratively, the region is divided into nine districts (Bibiani-Anhwiaso-Bekwai, Sefwi Wiawso, Aowin, Sefwi Akontombra, Suaman, Bodi, Juaboso, Bia West, and Bia East), which served as the clusters for our sampling framework, with 119 subdistricts. The region has 16 hospitals, 26 health centres, 31 clinics, 238 CHPS compounds, and 24 maternity homes, all contributing to public health services such as vaccinations [25]. Vaccination services are delivered through two primary channels: (1) facility-based appointments and (2) house-to-house campaigns supported by community volunteers.
Inclusion and exclusion criteria
The inclusion criteria for the study were:
- Persons eligible to receive the vaccine as prescribed by the Ghana Health Service, e.,15 years and above, including pregnant women, AND
- People who could read and/or understand local languages (Twi and/or Sefwi) or English AND
- People who had either not been vaccinated at all or had not received the full dose of any of the COVID-19 vaccines.
We excluded persons with cognitive or mental impairments, those who were severely ill during the data collection period or participants of a similar ongoing study.
Sample Size Determination
The required sample size was determined using the Cochran formula [31]:
\( N = \frac{Z^2 \, p \, q}{E^2} \)
Using a reliability confidence level of 95% (Z score of 1.96) and a 5% margin of error, an estimated sample size of 385 was calculated. Adjusting for a 15% non-response rate, as adopted by [16] yielded a minimum sample size of 443 participants. Four hundred and fifty (450) participants were eventually recruited for the study.
Sampling and data collection procedures
A multi-stage cluster sampling design was employed to ensure a representative sample across the region’s nine districts. This design was chosen to account for the dispersed and heterogeneous population distribution. All nine districts in the region were included in the study.
Stage one: Two sub-districts (clusters) were randomly selected from each of the nine districts using simple random sampling, yielding 18 clusters. This ensured proportional geographic representation at the district level.
Stage two: In each selected sub-district, one community was randomly selected.
Stage three: In each selected community, participants were chosen using a systematic sampling method with a random start, following the independent selection of clusters. Data collection commenced at a central, pre-identified location (the chief’s palace or, if absent, the assemblyman’s house). This method was applied consistently to all the selected communities to ensure uniformity. From this point, interviewers systematically selected every third household to the right (a sampling interval of k=3), a technique aimed at minimising selection bias and providing households with an equal chance of being chosen.
Within-household selection: In households with multiple eligible individuals, one respondent was selected using a lottery method (simple random sampling) to prevent interviewer selection bias.
Data collection continued in this manner within each selected community in each cluster until a target sample of 25 participants per community/ Subdistrict was reached. If necessary, the sampling extended to the nearest adjacent community to fulfil the quota, ensuring no cluster was underrepresented. The list of selected sub-districts is provided in Appendix A.
Variables
The dependent variable was vaccine hesitancy (yes/no). This was assessed by inquiring about participants’ COVID-19 vaccination status: vaccinated (ie, received at least 1 dose) vs unvaccinated. For analytical purposes, these responses were dichotomised into two categories: Non-hesitant (vaccinated) were participants who selected “Yes”, and hesitant (unvaccinated) were participants who selected “No”. This categorisation aligns with established research methodologies, where any indication of uncertainty or reluctance is classified as vaccine hesitancy. Such an approach is consistent with previous studies on vaccine acceptance and hesitancy [32].
The selection and the categorisation of the independent variables were guided by the WHO SAGE working group’s vaccine hesitancy determinant matrix [20]. This framework was chosen as it provides a comprehensive, internationally validated model of the multifaceted factors influencing vaccine uptake. This framework classifies determinants into two primary categories: contextual, individual and group influences, and vaccine/vaccination-specific issues. Given the unique circumstances of the COVID-19 pandemic, a fourth category, disease-specific influences, is also considered.
Individual influences (sociodemographic):
- Age: Participants’ ages were recorded and categorised into groups (e.g., 15–17 years, 18–25 years, etc.). Age can influence vaccine perceptions due to generational differences in health beliefs and information access.
- Gender: The study collected data on participants’ gender (male or female). Gender roles and norms within the community may affect health-seeking behaviours and vaccine acceptance.
- Education Status: Educational attainment was categorised (e.g., None, Primary, JHS, Secondary, Tertiary). Education level often correlates with health literacy, impacting understanding and acceptance of vaccination.
- Employment Status: Participants’ employment situations were noted (e.g., Government employed, Self-employed, Unemployed). Employment can influence access to health information and services, as well as perceptions of vaccine necessity.
- Marital Status: Marital status was recorded (e.g., Married, Single, Won’t say). Marital dynamics can affect decision-making processes regarding health interventions.
- Place of Residence: Participants’ living areas were classified (e.g., Urban, Peri-urban, Rural). Geographic location can impact vaccine accessibility and exposure to health campaigns.
Other variables
- Information on COVID-19 Vaccination: Participants were asked if they had received information about COVID-19 vaccination (Yes, No, ). Access to accurate information is crucial in shaping vaccine perceptions and addressing misconceptions.
- Sources of Information: The study identified where participants received their information (e.g., Radio, Television, Community Information Centres, social media). The credibility and nature of these sources can significantly influence vaccine attitudes.
- Religious Beliefs: The study considered the impact of religious beliefs on vaccine acceptance. Some religious doctrines or leaders may influence followers’ decisions regarding vaccination.
Vaccine/vaccination-specific issues:
- Reasons for Hesitancy
- Perceived Vaccine Side Effects: Concerns about potential side effects were documented. Personal or communal experiences with vaccine side effects can deter individuals from getting vaccinated.
- Perceived vaccine efficacy: Beliefs about the vaccine’s effectiveness were explored. Doubts about efficacy can lead to hesitancy or refusal.
- Trust in health staff administering the vaccine: Participants’ trust levels in healthcare providers were assessed. Trust in the competence and intentions of health workers can affect vaccine uptake.
- Preferred vaccination sites: Preferences for vaccination locations (e.g., Home visits, Health facilities, Workplaces) were recorded. Convenience and comfort with the vaccination setting can influence willingness to get vaccinated.
Data management and analysis
The dataset was cleaned in MS Excel. The cleaned dataset in an Excel spreadsheet named “final dataset” was imported into Stata version 14. All the variables were then encoded to assign variable labels and value labels for easy analysis.
Descriptive statistics were used to summarise the data and the demographic characteristics of the respondents. A multivariate logistic regression analysis test was run to assess the relationships between the socio-demographic characteristics and hesitancy towards the COVID-19 vaccines. Responses were compared for various socio-demographic characteristics by the dependent variable: vaccinated vs unvaccinated (hesitant), according to the vaccination hesitancy category as adopted by Chacón-Labrador et al. (2024) [32].
A total of 596 individuals were assessed for eligibility and approached for participation. Of these, 20 individuals (3.4%) declined to provide consent or assent and were excluded, resulting in 576 participants who were enrolled and interviewed.
Data cleaning and preparation were conducted on the dataset of 576 participants to ensure reliability for statistical analysis. This process identified 126 cases (21.9% of enrolled participants) with missing data for one or more variables critical to the planned multivariate regression. Given that the primary analysis required complete data for all covariates, a complete-case analysis (listwise deletion) was implemented [33], resulting in a final analytic sample of 450 participants. The pattern of missing data was reviewed and determined to be random and unsystematic, suggesting that its removal was unlikely to substantially bias the parameter estimates.
Ethical considerations:
The study received ethical clearance from the Ghana Health Service Ethics Review Committee (GHS-ERC) under reference number GHS-ERC 016/08/22. To safeguard privacy and confidentiality, all responses were collected anonymously. No identifying information (such as names, phone numbers, or addresses) was linked to the dataset. Participants were assigned unique codes to maintain anonymity and ensure secure data handling.
Results
Sociodemographic characteristics
Table 1 shows the background characteristics of study participants. The analysis included 450 eligible participants who reside in the Western North Region of Ghana. One-third of the respondents (149/450, 33.11%) were aged 15-24 years, and 145/450 (32.22%) were 25-29 years, with a median age of 29 years and an inter-quartile range ( Q3 (40) – Q1 (23)) of 17 years. The majority (277/450, 61.6%) of the respondents interviewed were females. In terms of the level of education, those without any formal education were 15.6% (70/450), while most had attained junior high school level, 36.2% (163/450), closely followed by secondary education, 25.5% (115/450). The majority of participants were self-employed (53.1%, 239/450), single (60.7%, 273/450), and living in rural areas (72.0%, 324/450) (Table 1).
Sixty per cent (271/450) of the respondents were hesitant to receive the COVID-19 vaccine. The bivariate analysis identified key sociodemographic factors associated with vaccine hesitancy. Employment status demonstrated a statistically significant association (p<0.001), with hesitancy as was educational (p = 0.035). Conversely, no statistically significant associations were found with age, gender, marital status, or place of residence (Table 2).
Sociodemographic factors associated with COVID-19 vaccine hesitancy
The multivariate logistic regression analysis (Table 3), adjusting for all other variables in the model, identified three factors as independent predictors of COVID-19 vaccine hesitancy. Compared to those with no formal education, the odds of hesitancy were significantly higher among respondents with a primary (aOR = 2.92; 95% CI: 1.37–6.22; p=0.006) or secondary (aOR = 2.17; 95% CI: 1.04–4.50; p=0.038) education.Conversely, self-employment was associated with significantly 40% reduced odds of hesitancy compared to being unemployed (aOR = 0.60; 95% CI: 0.38–0.93; p=0.021). Urban residence was also a significant protective factor, with urban dwellers having 36% lower odds of being hesitant than rural residents (aOR = 0.64; 95% CI: 0.40–1.00; p=0.049). Age, gender, marital status, and prior information on the vaccine were not independently associated with hesitancy in the final model (Table 3).
Reasons for rejecting the vaccine (hesitancy)
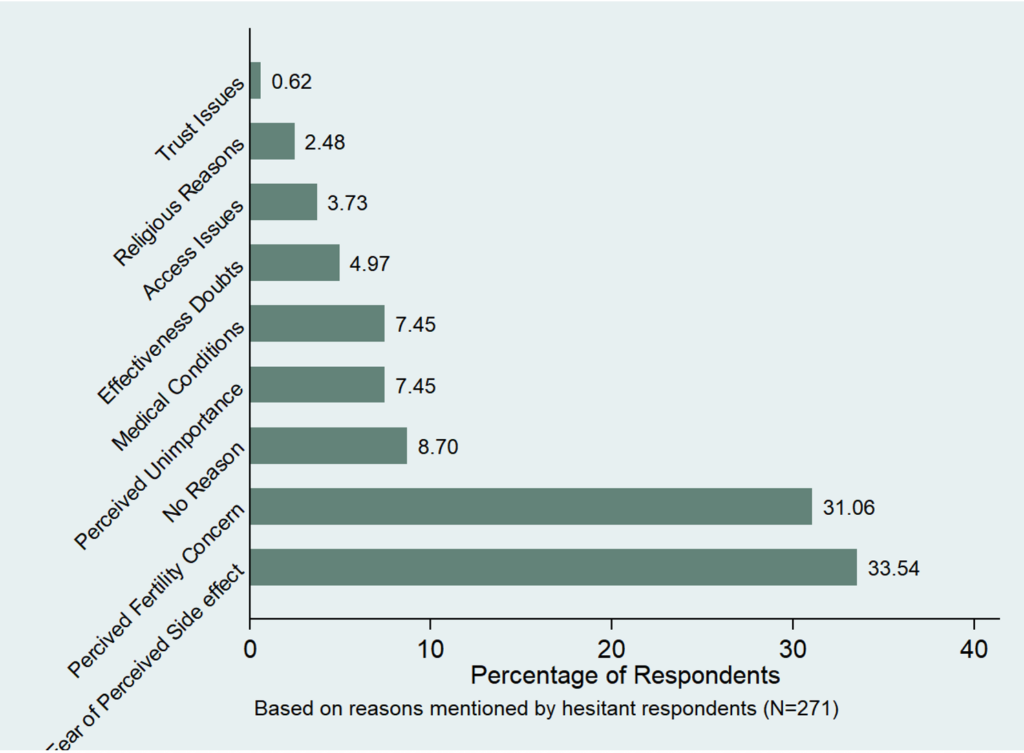
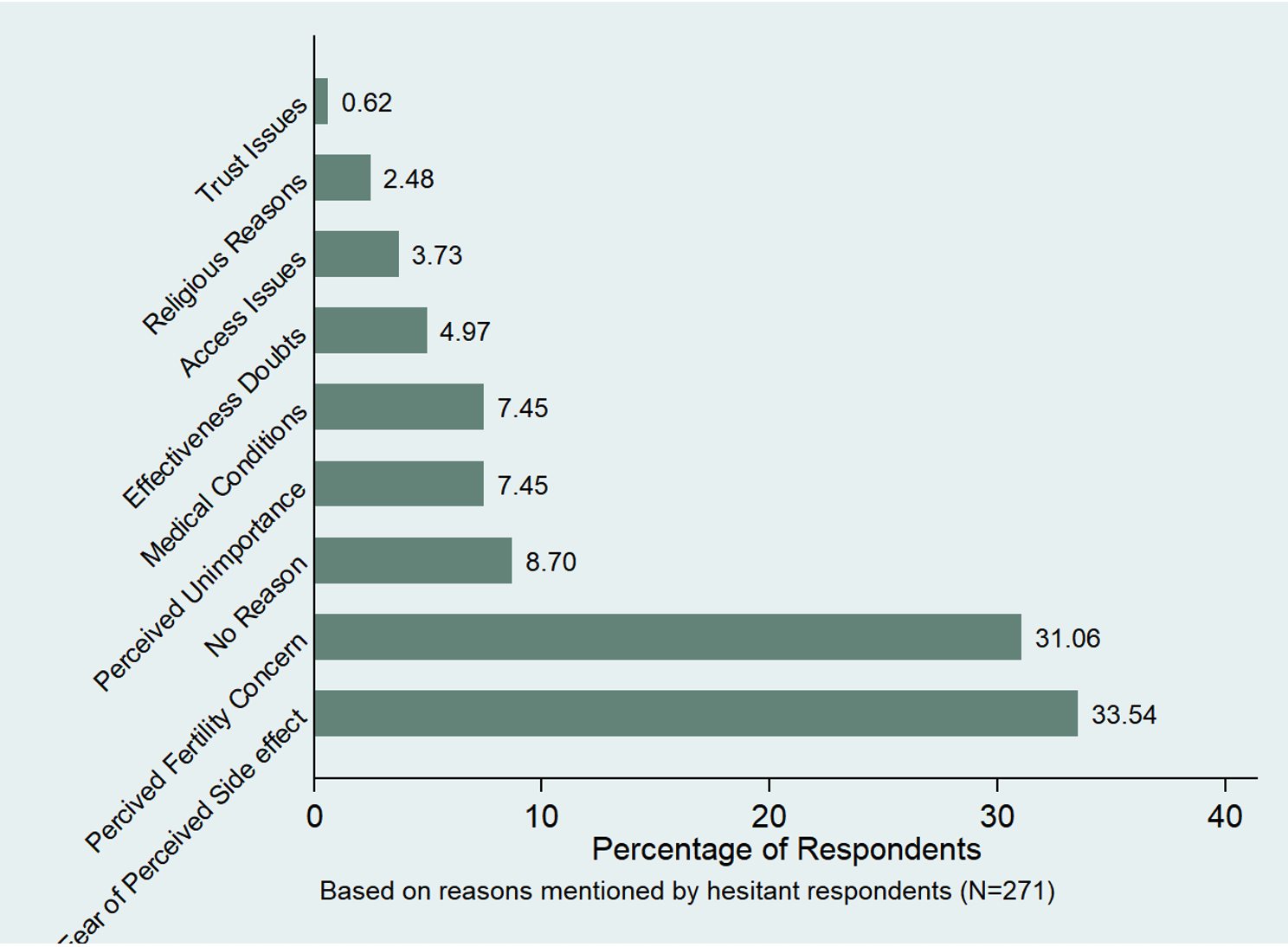
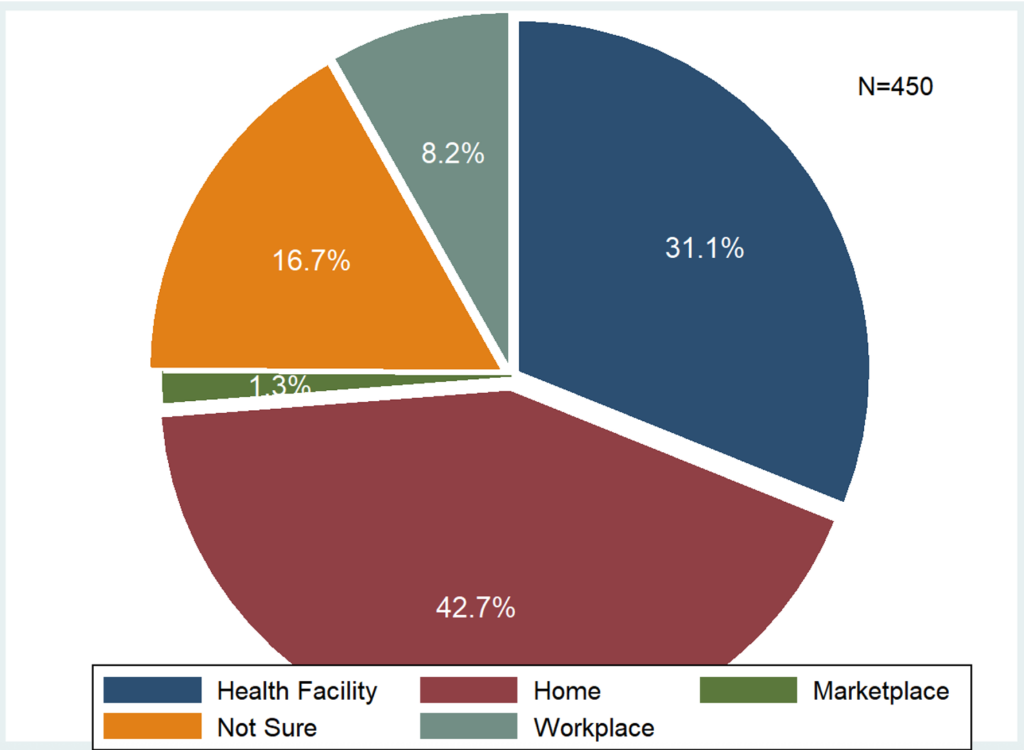
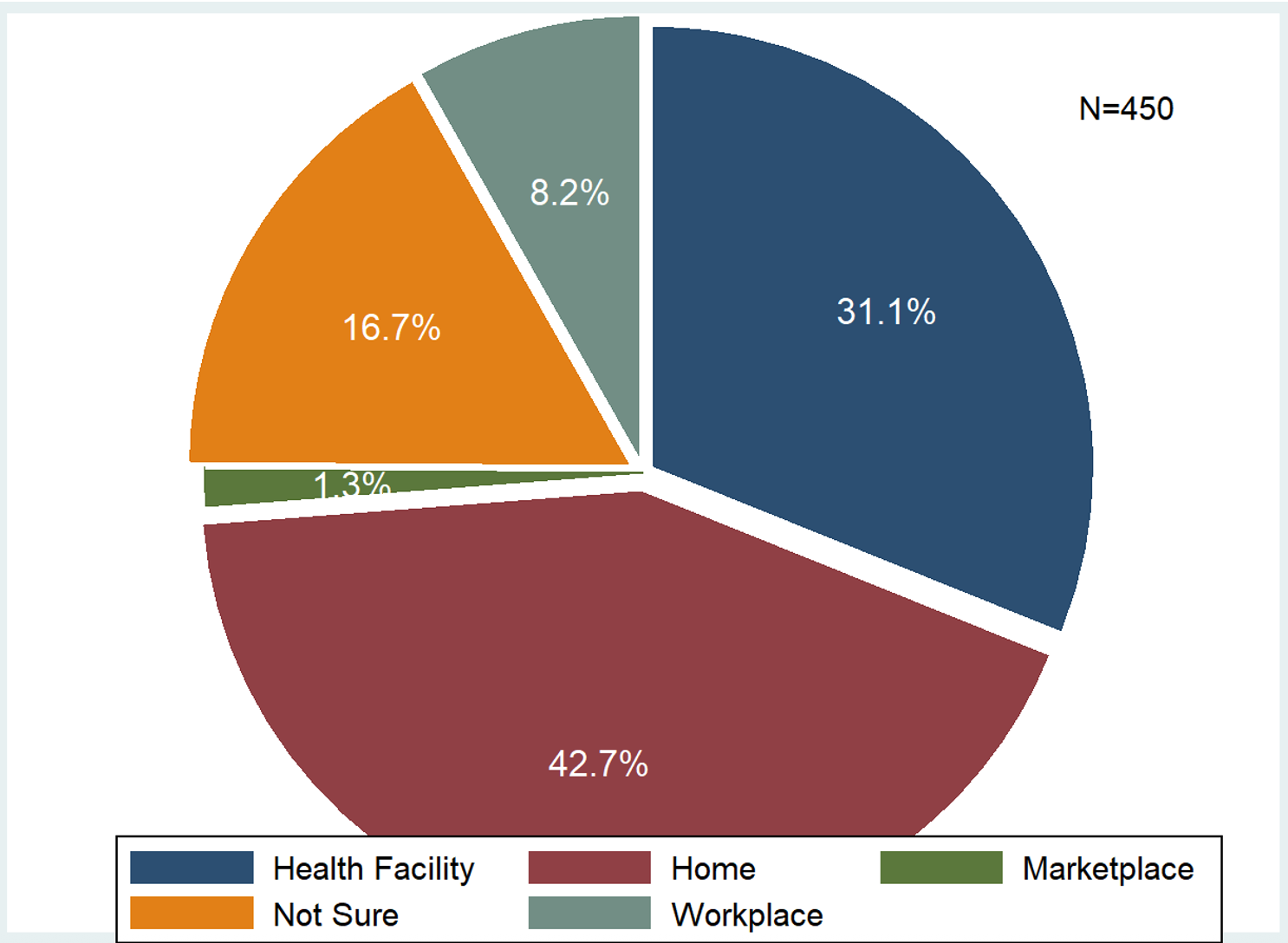
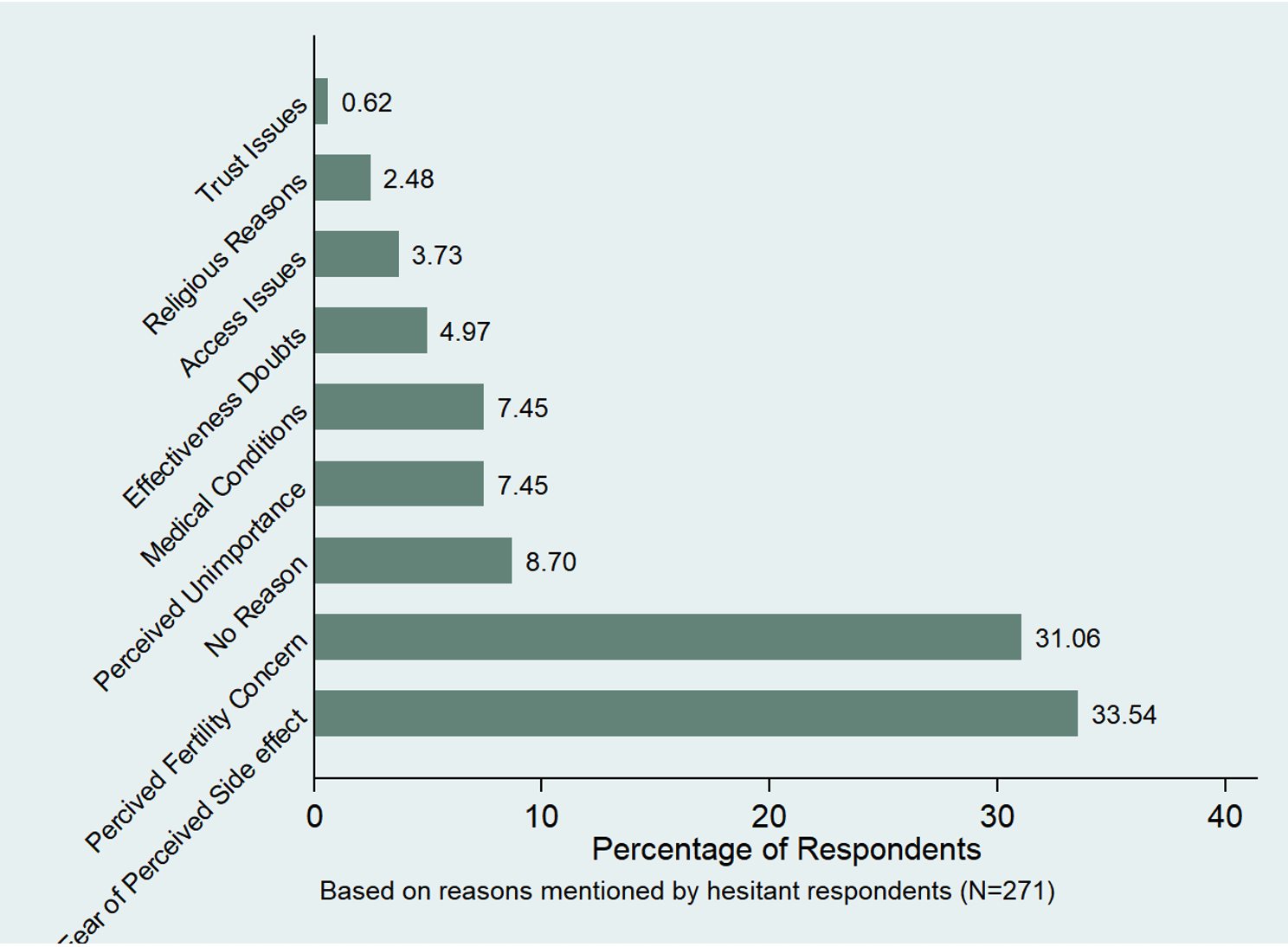
Regarding reasons for not taking the COVID-19 vaccine, approximately one-third (33.54%) of responses were attributed to concerns about the vaccine’s side effects. About 31% had concern or fear of inability to give birth after vaccination, while 8.7% of them had no reason for doing so. Less than 1% of them lack trust in health staff administering the vaccine, and about 2.4% attribute their hesitancy to religious beliefs (Figure 1).
Sources of information on COVID-19 vaccination
Almost all respondents (96.2%) had heard some information about the COVID-19 vaccination campaign (Figure 1), with television and radio stations being the major sources of information (67.90% and 20.32% respectively). One-on-one with health workers, family/friends and social media each constituted less than 5% of the sources of information (Figure 2).
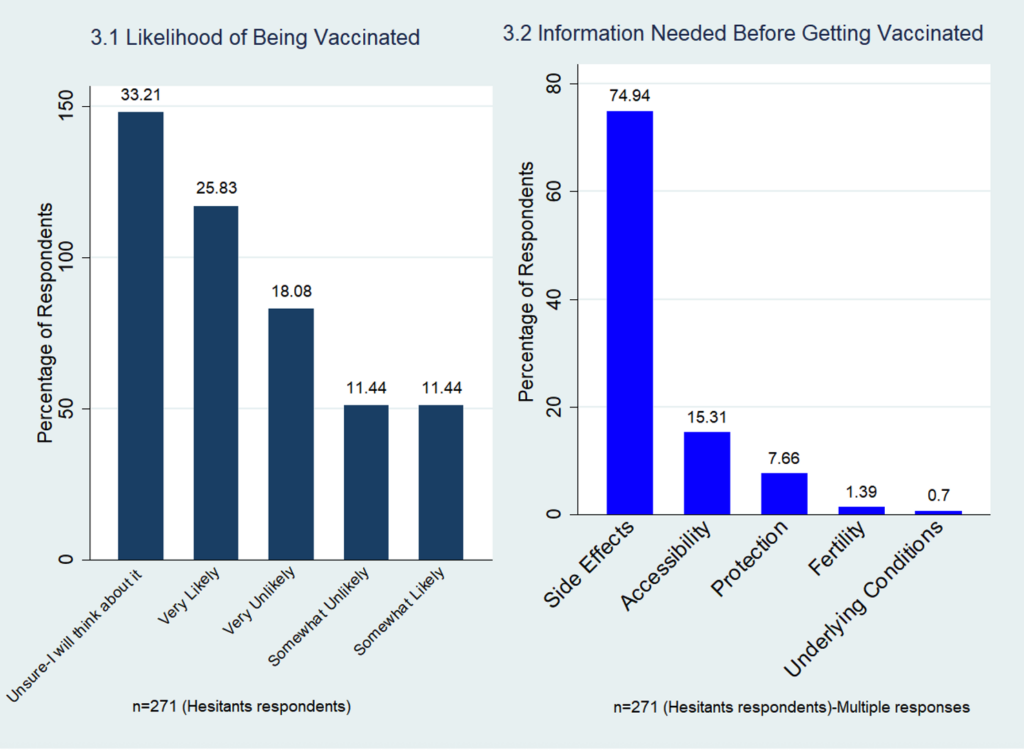
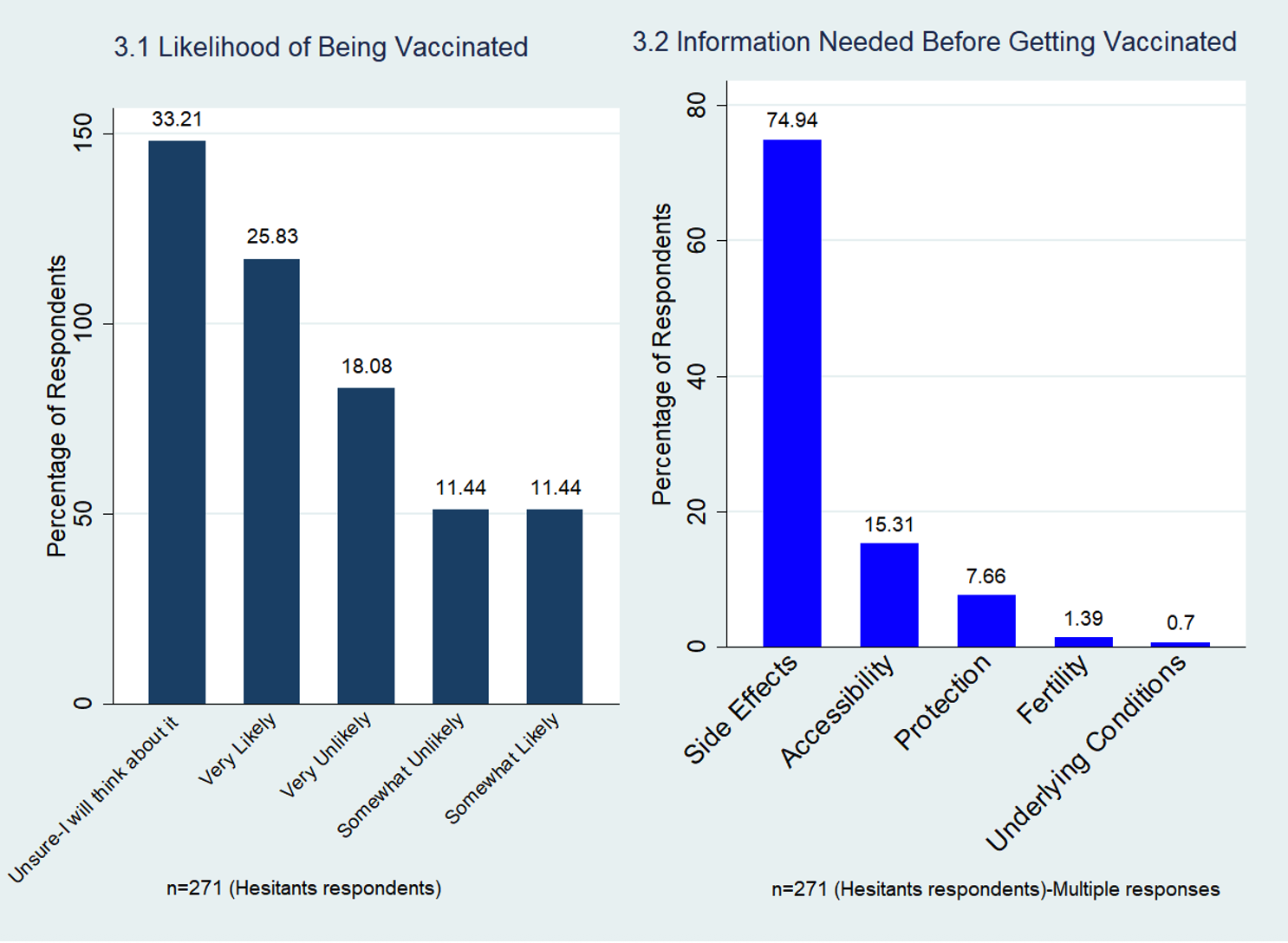
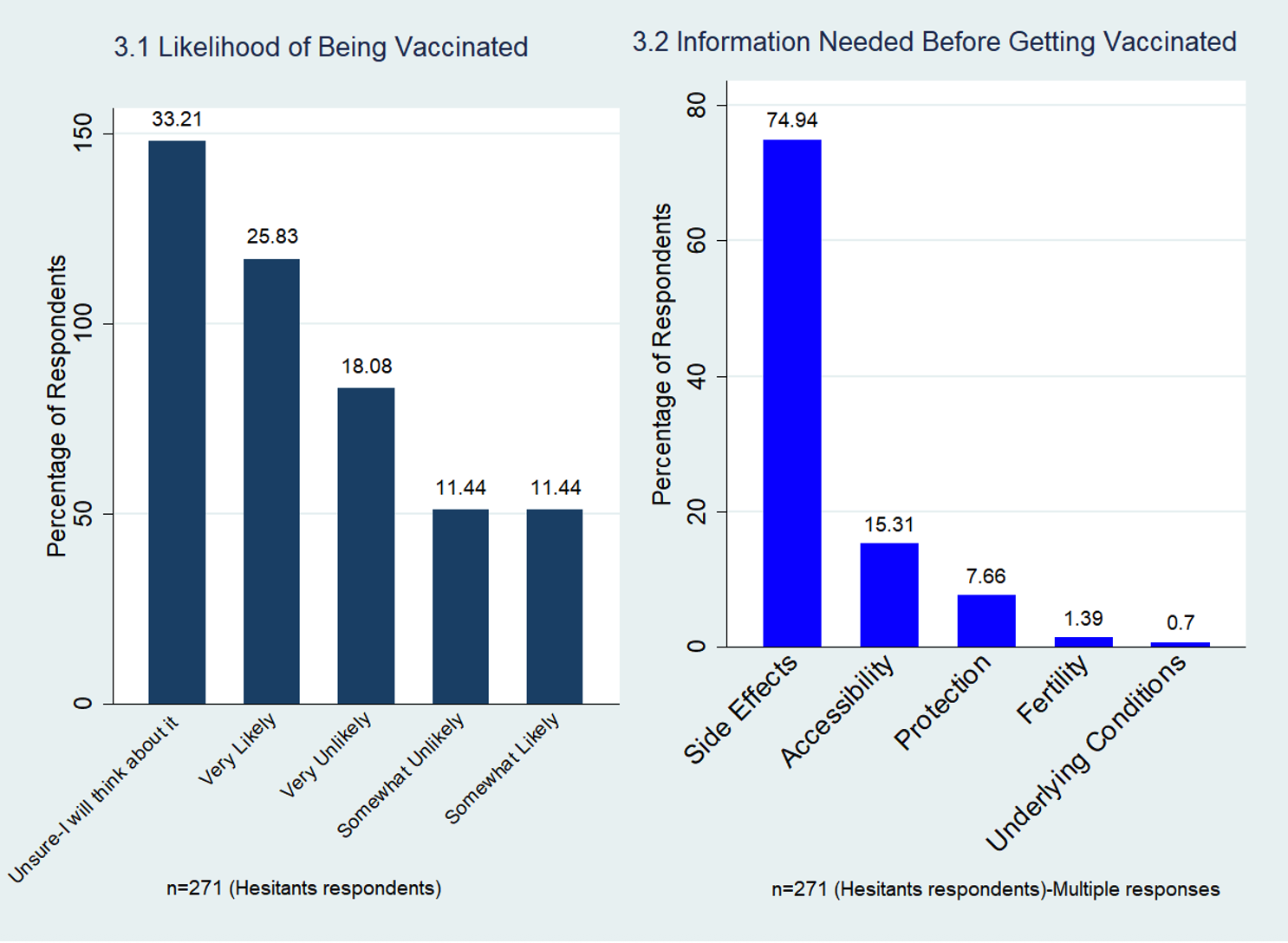
Likelihood of getting vaccinated and information that could potentially improve vaccine
Out of the total respondents, 25.83% (70/271) were very likely to accept the COVID-19 vaccine when it is made available to them, 11.44% (51/271) were somewhat likely while 33.21% (90/271) of them were not sure whether they would take the vaccine or not and 18.08% (49/271) were very unlikely to take the COVID-19 vaccine (Figure 3.1). When asked what information they would need which when provided, is likely to make them change their mind and decide to take the Covid-19 vaccines, respondents indicated the following: information on side effects (74.94%), accessibility of the vaccine (15.31%) and the whether the vaccine will be able to protect them (7.66%) or not, among others (Figure 3.2).
The largest proportion of the respondents (42.7%) preferred that health staff come to their homes to vaccinate them if vaccines were made available. However, nearly a third (31%) of the respondents are willing to visit health facilities to get vaccinated. Only a small fraction (8.2%) prefer vaccination at their workplaces (Figure 4).
Discussion
The study interviewed residents in the Western North Region, who had either not taken any of the COVID-19 vaccines at all or were partially vaccinated. This was quite surprising given that almost 70% of respondents were residents who had attained at least a junior high school level of education, and the popularity of the use of social media among this segment of the population (Table 2). Studies conducted by Seidu et al also found similar educational levels in their work [34].
The finding of the study, indicating a substantial majority of the study population had not received a single dose of the COVID-19 vaccine, which signifies high COVID-19 vaccine hesitancy in the Western North Region of Ghana. From the study, the main significant factors that contributed to vaccine hesitancy were education and employment status, which are similar to the findings by Seidu et al [34]. The majority of those who were not willing to take the vaccine were females. This prevalence is higher than the global average and highlights a critical public health challenge in the Region. These hesitancies are contributed to by numerous factors, ranging from personal/individual factors to culturally related factors. This finding moves the discussion beyond individual-level predictors to highlight a systemic issue, showing that achieving herd immunity in the Western North needs active interventions.
Employment status, a key determinant of financial accessibility, significantly influences health-seeking behaviour and serves as an enabling factor in healthcare utilisation, as proposed by Andersen’s behavioural model [35,36]. This is further reinforced by evidence linking economic engagement and urban infrastructure to increased access to health services and greater institutional trust, both of which are critical for vaccine acceptance. This study found that self-employed individuals demonstrated significantly lower odds of vaccine hesitancy compared to unemployed respondents. This may be attributed to the fact that self-employed individuals whose livelihoods depend directly on daily productivity and client interactions, vaccination may represent a strategic economic imperative rather than merely a health decision. The significant financial consequences of absence from work due to COVID-19-related illness or quarantine may outweigh potential convenience barriers, thereby motivating their vaccine uptake. This aligns with economic vulnerability theories, suggesting that individuals whose income is directly threatened by health disruptions show higher preventive health behaviours [37]. On the contrary, some previous literature, including Jafar et al. (2022) [38]which reported higher hesitancy among self-employed populations due to convenience barriers and Burke et. al (2020) [39] also indicated that most employers advised the employed population to be vaccinated following the intervention of working from home during the peak level of COVID-19, which therefore increased the chances of the employed population getting vaccinated compared to the unemployed and self-employed populations.
Understanding the reasons behind the rejection of COVID-19 vaccines is crucial for public health officials in their efforts to address vaccine hesitancy. In this study, we found that the primary reason for vaccine hesitancy was concern regarding potential side effects of the vaccine. This ties in with another finding from this study, which showed that the majority of the respondents would be convinced to take the vaccine if they had more information on the side effects of the vaccine. The link between concern about the potential side effects of the COVID-19 vaccines and hesitancy has been mentioned in several studies [6,8,9,11,12].
A minimal number of respondents attributed their refusal to vaccine effectiveness doubts and trust issues with the vaccine, which most likely shows that social mobilisation and education efforts of health staff in the region had reached a vast majority of the population. This finding aligns with evidence literature establishing that healthcare providers are one of the most trusted sources of health information and key influencers in vaccination decisions [40]. The primary reasons for hesitancy in this population appear to have shifted away from core issues of distrust and may be more closely aligned with other documented barriers [8,39]. Therefore, future public health efforts in similar contexts should maintain trust-building communication while tailoring interventions to address specific residual concerns like side-effect safety and disease risk perception.
Our findings show a high level of exposure to information on the COVID-19 vaccine among the study population. Most of this information was obtained from the traditional media channels of television and radio, with less than a negligible percentage coming directly from health providers. The near-universal penetration of COVID-19 vaccine messaging suggests that a lack of awareness was not a major factor in hesitancy in this population.
The analysis revealed that respondents who reported hearing information about the COVID-19 vaccine had lower odds of being vaccine-hesitant, although this association was not statistically significant. This trend aligns with the foundational health belief model and theories of health communication, which explain that access to information is a key precursor to adopting preventive health behaviours [40,41]. The point estimate suggests a potentially strong protective effect, where exposure to information could be associated with a reduction in hesitancy of more than 50%. The lack of statistical significance may be attributable to the relatively small number of respondents who had not heard the information, limiting the statistical power to detect a true effect. Nonetheless, the direction and magnitude of the association highlight the critical role of public health communication and social mobilisation campaigns. It implies that broadening the reach of accurate and accessible information remains a vital, though not singularly sufficient, strategy for mitigating vaccine hesitancy in the population.
While the reach of social mobilisation was good, it appears the messaging did not meet the expectations of the population to cause them to change their behaviours to accept the vaccine. It was established that the effectiveness of the social and behavioural change communication (SBCC) was questionable, as well as its contents. The communication was a mass information delivery on various communication channels, such as community information centres (CICs), Radio, Television, etc. (CICs), rather than a target group discussion to address the major concerns. change.
The multivariate analysis reveals that the relationship between sociodemographic factors and vaccine hesitancy is complex and often hidden in simpler analyses. After controlling for potential confounders, primary and secondary education emerged as a significant risk factor for hesitancy compared to those with no formal education. This finding was observed by the World Health Organisation (WHO) that higher education can, in a specific context, act as a barrier to acceptance [44]. This non-linear relationship suggests that the influence of education on health decision-making is complex and cannot be simply viewed as “more education equals less hesitancy”. This can be attributed to the fact that middle-level education may increase exposure to misinformation without conferring the critical appraisal skills needed to navigate conflicting claims and identify this misinformation. Contrary to our finding, the study conducted by Karp et al (2025) explains that higher levels of formal education predicted significantly greater willingness to receive the COVID-19 vaccine [45,46].
One positive finding from this study is that a significant minority were likely to change their minds (very likely and somewhat likely) and take the vaccine if they received enough information on the vaccine’s potential side effects and its ability to protect them. This suggests that a portion of the hesitant population’s refusal is not fixed but stems from a specific information deficit regarding safety and efficacy. This aligns with the work of Waszkiewicz et al (2022), which highlights previously vaccine-reluctant individuals’ concerns about their health and safety, and when this information is made available to them, they are likely to take the vaccine [48]. This finding, therefore, mandates public health officers to shift from broad awareness campaigns to targeted communication that addresses specific concerns about side effects and the effectiveness of the vaccine.
Also, some respondents were unsure whether they would take the vaccine or not (“Unsure-I will think about it”). This therefore implies that when there is an effective education (mobilisation), these groups of people are likely to change their minds and take the COVID-19 vaccine. This group of people are not outright refusers but in a state of indecision [49]. This aligns with the work by Quaife et al (2021) which highlighted that almost half of sampled population are willing to be vaccinated if the COVID-19 vaccine is made available to them [50].
The majority of such respondents who are willing to be vaccinated stated their preference to be vaccinated at home by health staff through house-to-house vaccinations. The strong preference for the house-to-to vaccinations highlights a barrier of convenience and accessibility. The preference for home-based administration suggests that factors such as distance to health facilities, travel costs, time taken off work, or the overall burden of accessing static vaccination sites are significant deterrents in this population. This aligns with the dimension of the ”3Cs” model of vaccine hesitancy in shaping vaccination behaviour [7]. To maximize vaccine coverage, public health strategies must not only address informational and perceptual barriers through communication but also systematically reduce physical access barriers by meeting people their doorsteps.
In our study, the majority of those who were not willing to take the vaccine were females; however, while being male had a negative association with vaccine hesitancy, it was not a statistically significant factor, in contrast to other studies [8,11,16,17]. Even though the proportion of respondents who expressed fear of inability to give birth after taking the vaccine may appear as an insignificant reason for its refusal, we think this concern of the women must not be ignored, especially since most of them wanted more information that would assure them that the vaccine would not affect their childbearing capacity before they could be convinced to take it.
The rich tapestry of cultural and ethnic diversity composition of the Western North Region mirrors the broader demographic landscape of Ghana, suggesting that findings from studies conducted in this region apply to other parts of the country. However, to enhance the robustness and generalizability of these conclusions, it is advisable for future research to include a more expansive and varied population across different settings. This approach will ensure that the insights gained are reflective of the nation’s diverse cultural and socioeconomic contexts
Limitations
One possible limitation of the study was not identifying whether hesitancy was towards a specific COVID-19 vaccine and any associated reasons for it. Another possible limitation of the study was its cross-sectional nature; it captures a specific moment in time, limiting the ability to assess changes in vaccine hesitancy over different phases of the pandemic. Self-reporting by the participants may have also introduced biases in the responses, such as social desirability bias. Another limitation of the study was that only sociodemographic variables were considered in the multivariate analysis.
Conclusion
The study highlights significant COVID-19 vaccine hesitancy in the Western North Region of Ghana, driven primarily by the interaction of sociodemographic, informational, perceptual factors and systemic factors. The multivariate analysis revealed a particularly detailed relationship between education and hesitancy, where primary and secondary education emerged as significant risk factors compared to no formal schooling, which may have been caused by increased exposure to misinformation without adequate critical validation. This is followed by employment type, where self-employed individuals show higher vaccine acceptance, and are likely driven by economic vulnerability. Furthermore, the study found that the main barrier to vaccination was not mainly opposition to the vaccine but rather specific concerns about perceived side effects and lack of information about the fertility impact and the protective benefit of the vaccine. While traditional media (radio, TV, CICs) were key information sources, these messages failed to address specific community concerns or foster behavioural change, highlighting the limitations of awareness-raising alone.
Targeted interventions addressing misinformation, emphasising vaccine safety and leveraging trusted community channels are essential to improving vaccine uptake. Despite hesitancy, a substantial proportion of respondents expressed willingness to vaccinate if provided with adequate information, emphasising the need for targeted public health campaigns to build confidence and achieve herd immunity.
Recommendations
To achieve the WHO recommended percentage of 60-70% of the population that has to be vaccinated to attain herd immunity, there is the need for targeted public health strategies, guide policy development and enhance engagement with health authorities to conduct regular and adequate education on COVID-19 infection and the benefits as well as potential side effects of vaccines against the disease especially among women in the region and religious leaders.
This will increase trust in residents towards the vaccines. Additionally, vaccination campaigns should focus more on house-to-house vaccinations to increase access to the vaccines. Health authorities, both at the regional and district levels, should also engage all relevant stakeholders during vaccination-related activities to improve the acceptability of residents towards the vaccines.
What is already known about the topic
- The influence of socio-economic variables such as age, education, and income to be associated with Covid-19 vaccine hesitancy.
- Mixed evidence on the effect of gender, education, and age in lower-middle-income countries (LMICs) on vaccine hesitancy [9].
- The influence of ethnicity has also been found to be a factor for vaccine hesitancy, while blacks or Africans were more vaccine hesitant compared to none-blacks.
What this study adds
- There is a need for the health authorities to conduct regular and adequate education on COVID-19 infection and the benefits, as well as the potential side effects of vaccines against the disease, especially among women in the region and religious leaders.
- Majority of the population is hesitant about the COVID-19 vaccine
- Primary and secondary education significantly increases the likelihood of vaccine-hesitant hesitant
- Self-employed individuals showed higher vaccine uptake to protect their livelihoods.
- Fear of potential side effects was the dominant reason for refusal.
- Gender was not found to be a significant factor for vaccine hesitancy.
- A sizable hesitant group remained persuadable with better safety information
- Urban residents are less likely to be hesitant compared to rural residents.
Acknowledgements
We sincerely acknowledge the efforts of the Public Health unit of the Regional Health Directorate and the district health directorate of the Western North Region for their dedicated efforts during the study period. We also acknowledge the efforts of the following people for their selfless dedication during the study period. Dr Francis Takyi (Sefwi Wiawso Municipal Health Directorate), Mr. Oheneba Oppong-Darko (Bibiani-Anhwiaso-Bekwai Municipal Health Directorate), Mr. Paul Noah Koam, (Suaman District Health Directorate) Mr. Abass Asigri (Bodi District Health Directorate), Mr. Konamsi Iddrisu (Bia East District Health Directorate), Mr. Cosmos Awortwi (Akontombra District Health Directorate) Miss Sathina Alipo (Juaboso District Health Directorate), Miss Rita Owusu (Aowin Municipal Health Directorate), Mr. James Badu (Sefwi Wiawso Municipal Health Directorate), Mr. Emmanuel Yirbuor S. (Juaboso District Health Directorate), Mr. Abraham Domo Koyaara (Sefwi Wiawso Municipal Health Directorate)
Authors´ contributions
Marion Okoh-Owusu, Billy Joshua, Kingsley Osei-Kwakye, Patrick Avevor Sally-Ann Ohene, Francis Chisaka Kasolo, Patrick Kuma-Aboagye and Osei Sakyi conceptualised the study, participated in its design and coordination, drafted the manuscript, initiated the research, interpreted the results, and drafted the final manuscript. Therson Mintah was involved in data collection, revised the methods, and guided the discussion and write-up of the manuscript. All authors read and approved the final manuscript.
| Characteristics | Number (Percent) |
|---|---|
| Age (years) | |
| 15–24 | 149 (33.11) |
| 25–29 | 145 (32.22) |
| 30–44 | 73 (16.22) |
| 45+ | 83 (18.44) |
| Gender | |
| Female | 277 (61.6) |
| Male | 173 (38.4) |
| Education | |
| Primary | 66 (14.7) |
| JHS | 163 (36.2) |
| Secondary | 115 (25.5) |
| Tertiary | 36 (8.0) |
| None | 70 (15.6) |
| Employment status | |
| Government employed | 22 (4.9) |
| Self-employed | 239 (53.1) |
| Unemployed | 189 (42.0) |
| Marital status | |
| Married | 176 (39.1) |
| Single | 273 (60.7) |
| Won’t say | 1 (0.2) |
| Income status | |
| Above GHC 2000 | 11 (2.4) |
| GHC 1000–2000 | 34 (7.6) |
| GHC 500–1000 | 81 (18.0) |
| Less than GHC 500 | 146 (32.4) |
| Won’t say | 178 (39.6) |
| Area of residence | |
| Rural | 324 (72.0) |
| Urban | 126 (28.0) |
| Variables | Hesitant 271 (60.22%) | Non-Hesitant 179 (39.78%) | p-value |
|---|---|---|---|
| Age | |||
| 15–24 | 84 (31.0) | 65 (36.31) | 0.518 |
| 25–34 | 93 (34.3) | 52 (29.05) | |
| 35–44 | 42 (15.49) | 31 (17.32) | |
| 45+ | 52 (19.19) | 31 (17.32) | |
| Gender | |||
| Female | 161 (59.41) | 116 (64.80) | 0.250 |
| Male | 110 (40.59) | 63 (35.20) | |
| Education Status | |||
| Primary | 33 (12.18) | 22 (12.18) | 0.035 |
| JHS | 100 (36.90) | 63 (35.20) | |
| Secondary | 68 (25.09) | 47 (26.26) | |
| Tertiary | 18 (6.64) | 18 (10.06) | |
| None | 52 (19.19) | 18 (10.06) | |
| Employment | |||
| Government employed | 7 (2.58) | 15 (8.38) | <0.001 |
| Self-employed | 162 (59.78) | 77 (43.02) | |
| Unemployed | 101 (37.64) | 87 (48.42) | |
| Marital Status | |||
| Married | 114 (42.07) | 65 (36.3) | 0.222 |
| Single | 157 (57.93) | 114 (63.7) | |
| Place of Residence | |||
| Rural | 187 (69.00) | 137 (76.54) | |
| Urban | 84 (31.01) | 42 (23.46) | |
| Information on COVID-19 Vaccination | |||
| Yes | 264 (97.42) | 168 (93.85) | 0.059 |
| No | 7 (2.58) | 11 (6.15) | |
| Variables | aOR (95% CI) | P-value |
|---|---|---|
| Age (years) | ||
| 15–24 | Ref | |
| 25–34 | 0.886 (0.523 – 1.501) | 0.652 |
| 35–44 | 1.314 (0.666 – 2.592) | 0.430 |
| 45+ | 1.230 (0.634 – 2.386) | 0.540 |
| Gender | ||
| Female | Ref | |
| Male | 0.726 (0.477 – 1.104) | 0.134 |
| Educational level | ||
| None | Ref | |
| JHS | 1.956 (0.992 – 3.857) | 0.053 |
| Primary | 2.917 (1.369 – 6.216) | 0.006 |
| Secondary | 2.167 (1.042 – 4.503) | 0.038 |
| Tertiary | 1.994 (0.713 – 5.578) | 0.188 |
| Employment status | ||
| Unemployed | Ref | |
| Government employed | 2.338 (0.765 – 7.147) | 0.136 |
| Self-employed | 0.596 (0.384 – 0.926) | 0.021 |
| Marital status | ||
| Married | Ref | |
| Single | 1.151 (0.723 – 1.832) | 0.555 |
| Area of residence | ||
| Rural | Ref | |
| Urban | 0.635 (0.404 – 0.997) | 0.049 |
| Hearing information on the COVID-19 vaccine | ||
| No | Ref | |
| Yes | 0.447 (0.160 – 1.254) | 0.126 |

References
- Mishra NP, Das SS, Yadav S, Khan W, Afzal M, Alarifi A, Kenawy ER, Ansari MT, Hasnain MS, Nayak AK. Global impacts of pre- and post-COVID-19 pandemic: focus on socio-economic consequences. Sensors International. 2020;1:100042. doi: 10.1016/j.sintl.2020.100042. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666351120300425.
- World Health Organization. Recommended composition of influenza virus vaccines for use in the 2020-2021 northern hemisphere influenza season. Geneva: WHO; 2020 Feb 28. 12 p. Available from: https://www.who.int/publications/m/item/recommended-composition-of-influenza-virus-vaccines-for-use-in-the-2020-2021-northern-hemisphere-influenza-season.
- Marzo RR, Sami W, Alam MZ, Acharya S, Jermsittiparsert K, Songwathana K, Pham NT, Respati T, Faller EM, Baldonado AM, Aung Y, Borkar SM, Essar MY, Shrestha S, Yi S. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Trop Med Health. 2022;50(1):4. doi: 10.1186/s41182-021-00393-1. Available from: https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-021-00393-1.
- De Gregorio E, Rappuoli R. From empiricism to rational design: a personal perspective of the evolution of vaccine development. Nat Rev Immunol. 2014;14(7):505-514. doi: 10.1038/nri3694. Available from: https://www.nature.com/articles/nri3694.
- Skwarczynski M, Toth I, editors. Micro- and nanotechnology in vaccine development. Oxford: William Andrew; 2017. 441 p. (Micro & Nano Technologies Series).
- MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dubé E, Gellin B, Goldstein S, Larson H, MacDonald N, Manzo ML, Reingold A, Tshering K, Zhou Y, Butler R, Duclos P, Guirguis S, Hickler B, Schuster M. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4164. doi: 10.1016/j.vaccine.2015.04.036. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X15005009.
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. Geneva: WHO; 2014 Nov 12. 63 p. Available from: https://www.who.int/docs/default-source/immunization/sage/2014/october/sage-working-group-revised-report-vaccine-hesitancy.pdf.
- Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245-251. doi: 10.1016/j.puhe.2021.02.025. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350621000834.
- Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, Syunyaev G, Malik AA, Aboutajdine S, Adeojo O, Anigo D, Armand A, Asad S, Atyera M, Augsburg B, Awasthi M, Ayesiga GE, Bancalari A, Björkman Nyqvist M, Borisova E, Bosancianu CM, Cabra García MR, Cheema A, Collins E, Cuccaro F, Farooqi AZ, Fatima T, Fracchia M, Galindo Soria ML, Guariso A, Hasanain A, Jaramillo S, Kallon S, Kamwesigye A, Kharel A, Kreps S, Levine M, Littman R, Malik M, Manirabaruta G, Mfura JLH, Momoh F, Mucauque A, Mussa I, Nsabimana JA, Obara I, Otálora MJ, Ouédraogo BW, Pare TB, Platas MR, Polanco L, Qureshi JA, Raheem M, Ramakrishna V, Rendrá I, Shah T, Shaked SE, Shapiro JN, Svensson J, Tariq A, Tchibozo AM, Tiwana HA, Trivedi B, Vernot C, Vicente PC, Weissinger LB, Zafar B, Zhang B, Karlan D, Callen M, Teachout M, Humphreys M, Mobarak AM, Omer SB. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27(8):1385-1394. doi: 10.1038/s41591-021-01454-y. Available from: https://www.nature.com/articles/s41591-021-01454-y.
- Stojanovic J, Boucher VG, Gagne M, Gupta S, Joyal-Desmarais K, Paduano S, Aburub AS, Sheinfeld Gorin SN, Kassianos AP, Ribeiro PAB, Bacon SL, Lavoie KL. Global trends and correlates of COVID-19 vaccination hesitancy: findings from the iCARE study. Vaccines. 2021;9(6):661. doi: 10.3390/vaccines9060661. Available from: https://www.mdpi.com/2076-393X/9/6/661.
- Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. 2021;9:698111. doi: 10.3389/fpubh.2021.698111. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2021.698111/full.
- Ackah BBB, Woo M, Stallwood L, Fazal ZA, Okpani A, Ukah UV, Adu PA. COVID-19 vaccine hesitancy in Africa: a scoping review. Glob Health Res Policy. 2022;7(1):21. doi: 10.1186/s41256-022-00255-1. Available from: https://ghrp.biomedcentral.com/articles/10.1186/s41256-022-00255-1.
- Parimi K, Gilkeson K, Creamer BA. COVID-19 vaccine hesitancy: considerations for reluctance and improving vaccine uptake. Hum Vaccin Immunother. 2022;18(5):2062972. doi: 10.1080/21645515.2022.2062972. Available from: https://www.tandfonline.com/doi/full/10.1080/21645515.2022.2062972.
- Brackstone K, Atengble K, Head MG, Boateng LA. COVID-19 vaccine hesitancy in Ghana: the roles of political allegiance, misinformation beliefs, and sociodemographic factors. medRxiv. 2022. doi: 10.1101/2022.03.16.22272463. Preprint. Available from: http://medrxiv.org/lookup/doi/10.1101/2022.03.16.22272463.
- Ghana Health Service. DHIMS 2. Accra: Ghana Health Service. Available from: https://dhims.chimgh.org/dhims/dhis-web-login/.
- Acheampong T, Akorsikumah EA, Osae-Kwapong J, Khalid M, Appiah A, Amuasi JH. Examining vaccine hesitancy in sub-Saharan Africa: a survey of the knowledge and attitudes among adults to receive COVID-19 vaccines in Ghana. Vaccines. 2021;9(8):814. doi: 10.3390/vaccines9080814. Available from: https://www.mdpi.com/2076-393X/9/8/814.
- Alhassan RK, Aberese-Ako M, Doegah PT, Immurana M, Dalaba MA, Manyeh AK, Klu D, Acquah E, Ansah EK, Gyapong M. COVID-19 vaccine hesitancy among the adult population in Ghana: evidence from a pre-vaccination rollout survey. Trop Med Health. 2021;49(1):96. doi: 10.1186/s41182-021-00357-5. Available from: https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-021-00357-5.
- Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165-4175. doi: 10.1016/j.vaccine.2015.04.037. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X15005010.
- Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, Eskola J, Liang X, Chaudhuri M, Dubé E, Gellin B, Goldstein S, Larson H, MacDonald N, Manzo ML, Reingold A, Tshering K, Zhou Y, Butler R, Duclos P, Guirguis S, Hickler B, Schuster M. Strategies for addressing vaccine hesitancy – a systematic review. Vaccine. 2015;33(34):4180-4190. doi: 10.1016/j.vaccine.2015.04.040. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X15005046.
- World Health Organization. Summary WHO SAGE conclusions and recommendations on vaccine hesitancy. Geneva: WHO; 2015 Jan. 5 p.
- Roy DN, Biswas M, Islam E, Azam MS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: a systematic review. Delcea C, editor. PLoS One. 2022;17(3):e0265496. doi: 10.1371/journal.pone.0265496. Available from: https://dx.plos.org/10.1371/journal.pone.0265496.
- Rahbeni TA, Satapathy P, Itumalla R, Marzo RR, Mugheed KAL, Khatib MN, Gaidhane S, Zahiruddin QS, Rabaan AA, Alrasheed HA, Al-Subaie MF, Al Kaabil NA, Alissa M, Ibrahim AAAL, Alsaif HA, Naser IH, Rustagi S, Kukreti N, Dziedzic A. COVID-19 vaccine hesitancy: umbrella review of systematic reviews and meta-analysis. JMIR Public Health Surveill. 2024;10:e54769. doi: 10.2196/54769. Available from: https://publichealth.jmir.org/2024/1/e54769. Erratum in: JMIR Public Health Surveill. 2024;10:e64080. doi: 10.2196/64080.
- Pires C. Global predictors of COVID-19 vaccine hesitancy: a systematic review. Vaccines. 2022;10(8):1349. doi: 10.3390/vaccines10081349. Available from: https://www.mdpi.com/2076-393X/10/8/1349.
- United Nations Children’s Fund, UNICEF Office for the Eastern Caribbean Area, Caribbean Development Research Services Inc. COVID-19 vaccine hesitancy survey report 2021. Hastings: UNICEF; 2021 Dec. 54 p. Available from: https://www.unicef.org/easterncaribbean/reports/covid-19-vaccine-hesitancy-survey-report-2021.
- Okoh-Owusu M, Billy J, Dapaa S, Avevor P, Sakyi O, Twum-Andoh S, Sawadigo SA, Kwadzodeh EF, Kotey MA, Issahaku GR, Salifu S, Osei-Kwakye K, Laryea D, Bekoe FA. Against the clock: effect of late detection of a mumps outbreak in the Western North Region of Ghana, 2022. J Interv Epidemiol Public Health. 2025;8(1):13. doi: 10.37432/jieph-d-24-02036. Available from: https://afenet-journal.org/against-the-clock-effect-of-late-detection-of-a-mumps-outbreak-in-the-western-north-region-of-ghana-2022/.
- Ofori OB, Frimpong JA, Baffoe-Nyarko I, Abdul-Tawab A, Gudjinu HY, Laryea EB, Okoh-Owusu M, Kenu E, Laryea DO, Asiedu-Bekoe F. Factors influencing the achievement of core acute flaccid paralysis indicators in the Western North Region, Ghana, 2022. J Interv Epidemiol Public Health. 2025;8(3):46. doi: 10.37432/jieph.2025.8.3.170. Available from: https://afenet-journal.org/factors-influencing-the-achievement-of-core-acute-flaccid-paralysis-indicators-in-the-western-north-region-ghana-2022/.
- Ghana Statistical Service. Ghana 2021 population and housing census: general report volume 3A. Accra: GSS; 2022. p. 32.
- World Bank Group. Climate risk profile: Ghana. Washington, DC: World Bank Group; 2021. 28 p. Available from: https://climateknowledgeportal.worldbank.org/sites/default/files/country-profiles/15857-WB_Ghana%20Country%20Profile-WEB.pdf.
- Ministry of Health. 2021 holistic assessment report. Accra: MoH; 2022 Apr. 56 p. Available from: https://www.moh.gov.gh/wp-content/uploads/2022/08/2021-Holistic-Assessment-Report_v1.7.3.pdf.
- National Commission on Culture. Western North Region. Accra: NCC; 2025. Available from: https://ghanaculture.gov.gh/western-north/.
- Daniel WW. Biostatistics: a foundation for analysis in the health sciences. 4th ed. New York: Wiley; 1987. 734 p. (Wiley series in probability and mathematical statistics. Applied probability and statistics).
- Chacón-Labrador FR, Passantino MG, Moncada-Ortega A, Ávila AA, Moreno AA, Kuffaty-Akkou NA, Pedroza LM, Camejo-Ávila NA, Mendoza-Millán DL, Rodriguez-Saavedra CM, Marcano-Rojas MV, Hernández-Medina F, Grillet ME, Carrión-Nessi FS, Forero-Peña DA. Understanding the factors associated with COVID-19 vaccine hesitancy in Venezuela. BMC Public Health. 2024;24(1):1117. doi: 10.1186/s12889-024-18598-4. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-18598-4.
- Ranganathan P, Hunsberger S. Handling missing data in research. Perspect Clin Res. 2024;15(2):99-101. doi: 10.4103/picr.picr_38_24. Available from: https://journals.lww.com/picr/fulltext/2024/15020/handling_missing_data_in_research.7.aspx.
- Seidu A, Ampomah IG, Emeto TI. COVID-19 vaccine uptake and associated factors among persons with disabilities in Ghana’s Ashanti Region. Health Sci Rep. 2024;7(12):e70210. doi: 10.1002/hsr2.70210. Available from: https://onlinelibrary.wiley.com/doi/10.1002/hsr2.70210.
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10. doi: 10.2307/2137284. Available from: https://www.jstor.org/stable/2137284.
- Alkhawaldeh A, AlBashtawy M, Rayan A, Abdalrahim A, Musa A, Eshah N, Khait AA, Qaddumi J, Khraisat O, AlBashtawy S. Application and use of Andersen’s behavioral model as theoretical framework: a systematic literature review from 2012–2021. Iran J Public Health. 2023;52(7):1326-1334. doi: 10.18502/ijph.v52i7.13236. Available from: https://publish.kne-publishing.com/index.php/ijph/article/view/13236.
- Skaathun B, Rodríguez-Rosales CI, Gahbler-Lopez G, Furtwengler SR, Salgin L, Muñoz FA, Smith DM, Stockman JK, O’Bryan SE, Ramirez D, James-Price C, Servin AE. Vaccine hesitancy and economic hardship: a latent class analysis of racial and ethnic minority communities at high risk of COVID-19 infection in Southern California. Hum Vaccin Immunother. 2025;21(1):2529612. doi: 10.1080/21645515.2025.2529612. Available from: https://www.tandfonline.com/doi/full/10.1080/21645515.2025.2529612.
- Jafar A, Dambul R, Dollah R, Sakke N, Mapa MT, Joko EP. COVID-19 vaccine hesitancy in Malaysia: exploring factors and identifying highly vulnerable groups. Mittal P, editor. PLoS One. 2022;17(7):e0270868. doi: 10.1371/journal.pone.0270868. Available from: https://dx.plos.org/10.1371/journal.pone.0270868.
- Burke PF, Masters D, Massey G. Enablers and barriers to COVID-19 vaccine uptake: an international study of perceptions and intentions. Vaccine. 2021;39(36):5116-5128. doi: 10.1016/j.vaccine.2021.07.056. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X21009476.
- Tuckerman J, Kaufman J, Danchin M. Effective approaches to combat vaccine hesitancy. Pediatr Infect Dis J. 2022;41(5):e243-e245. doi: 10.1097/INF.0000000000003499. Available from: https://journals.lww.com/pidj/Abstract/2022/05000/Effective_Approaches_to_Combat_Vaccine_Hesitancy.18.aspx.
- Pourrazavi S, Fathifar Z, Sharma M, Allahverdipour H. COVID-19 vaccine hesitancy: a systematic review of cognitive determinants. Health Promot Perspect. 2023;13(1):21-35. doi: 10.34172/hpp.2023.03. Available from: https://hpp.tbzmed.ac.ir/Article/hpp-41159.
- Alyafei A, Easton-Carr R. The health belief model of behavior change. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [updated 2024 May 19]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK606120/.
- Mahindarathne PP. Assessing COVID-19 preventive behaviours using the health belief model: a Sri Lankan study. J Taibah Univ Med Sci. 2021;16(6):914-919. doi: 10.1016/j.jtumed.2021.07.006. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1658361221001438.
- World Health Organization. Vaccine hesitancy: a growing challenge for immunization programmes. Geneva: WHO; 2015 Aug 18. Available from: https://www.who.int/news/item/18-08-2015-vaccine-hesitancy-a-growing-challenge-for-immunization-programmes.
- Karp SR, Jean YB, Ashiru OA, Rangrej SB. COVID-19 vaccine willingness and education level: a multinational cross-sectional analysis. Cureus. 2025;17(6):e85544. doi: 10.7759/cureus.85544. Available from: https://www.cureus.com/articles/373000-covid-19-vaccine-willingness-and-education-level-a-multinational-cross-sectional-analysis.
- Vardavas C, Nikitara K, Aslanoglou K, Lagou I, Marou V, Phalkey R, Leonardi-Bee J, Fernandez E, Vivilaki V, Kamekis A, Symvoulakis E, Noori T, Wuerz A, Suk JE, Deogan C. Social determinants of health and vaccine uptake during the first wave of the COVID-19 pandemic: a systematic review. Prev Med Rep. 2023;35:102319. doi: 10.1016/j.pmedr.2023.102319. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2211335523002103.
- Lamptey E, Serwaa D, Appiah AB. A nationwide survey of the potential acceptance and determinants of COVID-19 vaccines in Ghana. Clin Exp Vaccine Res. 2021;10(2):183-190. doi: 10.7774/cevr.2021.10.2.183. Available from: https://ecevr.org/DOIx.php?id=10.7774/cevr.2021.10.2.183.
- Waszkiewicz P, Lewulis P, Górski M, Czarnecki A, Feleszko W. Public vaccination reluctance: what makes us change our minds? Results of a longitudinal cohort survey. Vaccines. 2022;10(7):1081. doi: 10.3390/vaccines10071081. Available from: https://www.mdpi.com/2076-393X/10/7/1081.
- Bussink-Voorend D, Hautvast JLA, Vandeberg L, Visser O, Hulscher MEJL. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav. 2022;6(12):1634-1648. doi: 10.1038/s41562-022-01431-6. Available from: https://www.nature.com/articles/s41562-022-01431-6.
- Quaife M, Torres-Rueda S, Dobreva Z, Van Zandvoort K, Jarvis CI, Gimma A, Zulfiqar W, Khalid M, Vassall A. COVID-19 vaccine hesitancy and social contact patterns in Pakistan: results from a national cross-sectional survey. BMC Infect Dis. 2023;23(1):321. doi: 10.1186/s12879-023-08305-w. Available from: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08305-w.
