Research | Open Access | Volume 9 (1): Article 30 | Published: 18 Feb 2026
Epidemiology of measles infection in Namibia, 2020-2024
Menu, Tables and Figures
Navigate this article
Tables
| Characteristics | Frequency (n=75) | Percentage (%) |
|---|---|---|
| Sex | ||
| Female | 32 | 42.7 |
| Male | 43 | 57.3 |
| Place of residence | ||
| Urban | 30 | 40.0 |
| Rural | 45 | 60.0 |
| Age (years) | ||
| 0–4 | 38 | 50.7 |
| 5–9 | 28 | 37.3 |
| 10–14 | 4 | 5.3 |
| 15–19 | 4 | 5.3 |
| 20+ | 1 | 1.3 |
| Vaccination status | ||
| Not Vaccinated | 12 | 16.0 |
| Vaccinated | 33 | 44.0 |
| Unknown | 30 | 40.0 |
| Number of vaccine doses | ||
| Vaccinated 1st dose | 15 | 20.0 |
| Vaccinated 2nd dose | 18 | 24.0 |
| Not vaccinated | 12 | 16.0 |
| Unknown vaccination status | 30 | 40.0 |
Table 1: Distribution of measles cases by sex, age, rural/ urban setting and vaccination status in Namibia 2020-2024
| Age group | Vaccination status | Total | ||
|---|---|---|---|---|
| Vaccinated n (%) | Not vaccinated n (%) | Unknown vaccination status n (%) | ||
| 0–4 | 19 (50.0) | 7 (18.4) | 12 (31.6) | 38 |
| 5–9 | 11 (39.0) | 3 (10.7) | 14 (50.0) | 28 |
| 10–14 | 1 (25.0) | 1 (25.0) | 2 (50.0) | 4 |
| 15–19 | 2 (50.0) | 1 (25.0) | 1 (25.0) | 4 |
| 20+ | 0 (0) | 0 (0.0) | 1 (100) | 1 |
Table 2: Distribution of measles infections by age group and vaccination status in Namibia, 2020-2024
| Variable | Incidence rates 2020 | Incidence rates 2021 | Incidence rates 2022 | Incidence rates 2023 | Incidence rates 2024 |
|---|---|---|---|---|---|
| Age group | |||||
| 0–4 | 0.96 | 0.24 | 2.89 | 3.61 | 1.92 |
| 5–9 | 0.79 | 0.00 | 1.58 | 1.84 | 3.16 |
| 10–14 | 0.00 | 0.00 | 0.31 | 0.00 | 0.92 |
| 15–19 | 1.40 | 0.00 | 0.00 | 1.08 | 0.36 |
| 20+ | 0.01 | 0.06 | 0.00 | 0.00 | 0.00 |
| Gender | |||||
| Male | 2.90 | 0.27 | 0.07 | 1.15 | 0.81 |
| Female | 2.10 | 0.06 | 0.71 | 0.52 | 0.78 |
Table 3: Measles Incidence rates/100000 population in Namibia, 2020-2024
Figures
Keywords
- Measles
- Epidemiology
- Namibia
Monika Densi1,2,3,&, Ndeshihafela Sakaria1,2, Diana Ewaga 2,3, Secilia Nghidishange2, Silas Nghishihange1,2, Shalo Nelly Ntusi1
1Ministry of Health and Social Services, Health Information and Research Directorate, Windhoek, Namibia, 2Namibia Field Epidemiology and Laboratory Training Programme, Windhoek, Namibia, 3University of Namibia, Department of Public Health, Oshakati, Namibia
&Corresponding author: Monika Densi, Namibia Field Epidemiology and Laboratory Training Program, Email: monicadensy@gmail.com, ORCID: https://orcid.org/0009-0009-7217-7722
Received: 25 May 2025, Accepted: 16 Feb 2026, Published: 18 Feb 2026
Domain: Infectious Disease Epidemiology
Keywords: Measles, epidemiology, Namibia
©Measles, Epidemiology, Namibia et al. Journal of Interventional Epidemiology and Public Health (ISSN: 2664-2824). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Monika Densi et al., Epidemiology of measles infection in Namibia, 2020-2024. Journal of Interventional Epidemiology and Public Health. 2026; 9(1):30. https://doi.org/10.37432/jieph-d-25-00117
Abstract
Introduction: Despite efforts towards measles elimination, Namibia continues to report outbreaks and cases of measles. The World Health Organization estimates that 9.6 million measles cases and 128,000 deaths were reported worldwide in 2019, 50% of which occurred in Africa alone. Namibia reported 75 cases and 0 deaths in the past five years from 2020 to 2024. We described the epidemiology of measles infection in Namibia from 2020 to 2024.
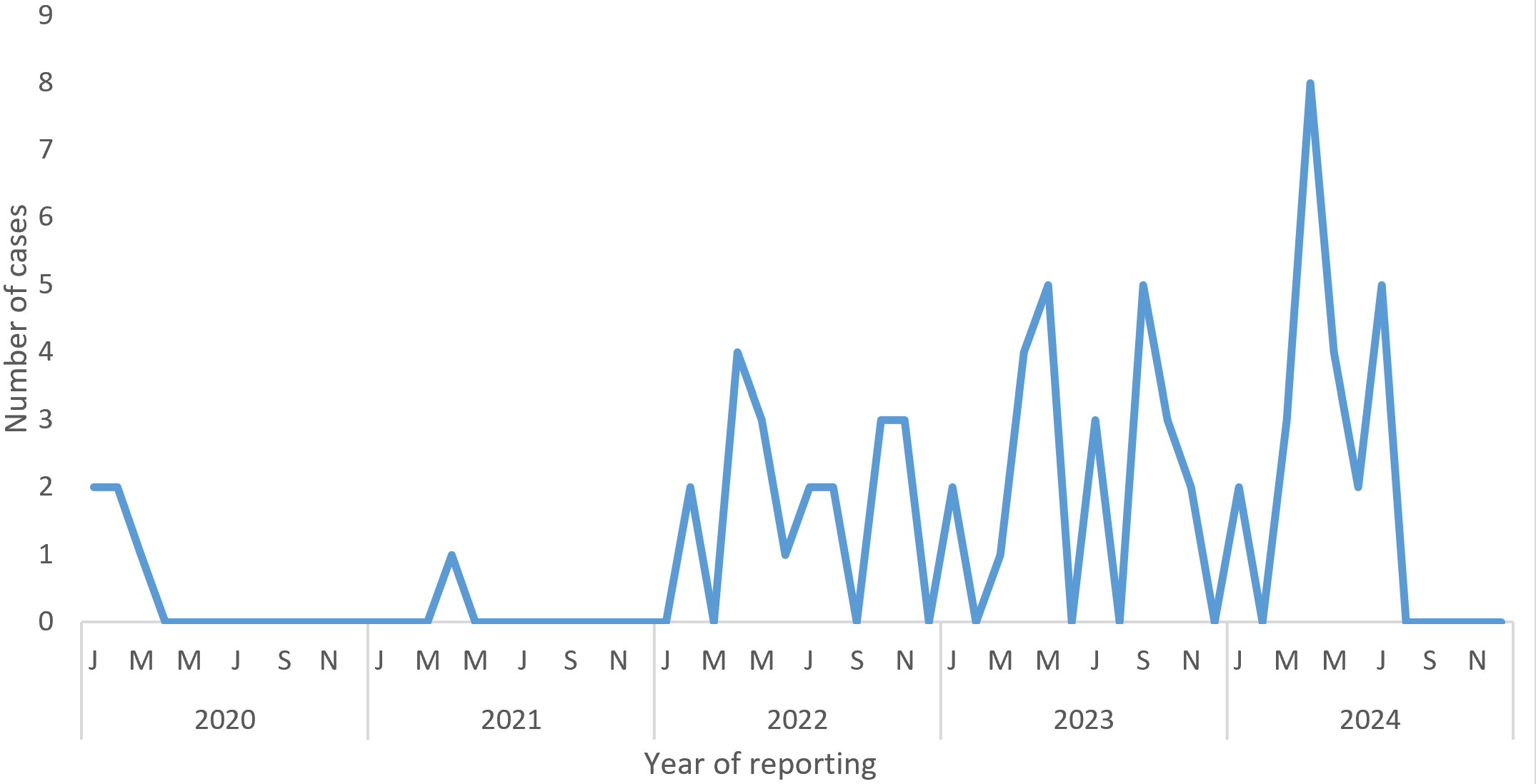
Methods: A retrospective secondary data analysis of measles infections reported in the national measles line list between January 2020 and April 2024 was conducted. We calculated frequencies, incidence rates, proportions, and time series to identify trends and seasonality. Data were cleaned in Microsoft Excel and analysed in SPSS version 25 and Datawrapper. The data were visualised using tables, graphs, and maps.
Results: A total of 75 cases recorded in the national measles line list between January 2020 and April 2024 were analysed in this study. The median age was 5 (Interquartile range: 2.5 – 9) years. Half of the cases (50.1%) were aged 0-4 years old. There was a steady increase in measles incidence in Namibia, with a rate of 0.73 per 100,000 in 2024 (0.73/100,000). A seasonal trend was observed, with most cases occurring between April and May of each year. Among the cases, 44% were vaccinated, 40% had unknown vaccination status, and 16% were unvaccinated. The highest incidence rates were reported in the Erongo region in 2024 (6.24/100,000), followed by those in the northern regions.
Conclusion: The burden of measles infections was observed among children aged 0-4 years, and during the winter season. With a steady increase in the number of cases in the country, measures for successful elimination need to be strengthened to prevent outbreaks and ensure that Namibia remains on track with its elimination targets.
Introduction
An estimated 9.6 million measles cases and 128,000 deaths were reported worldwide in 2019, of which Africa accounted for more than 50% [1]. Measles cases continue to rise despite elimination measures such as mass vaccination campaigns and strengthening surveillance systems to detect cases early and provide rapid responses to outbreaks. Sub-Saharan Africa has recently experienced a surge in measles infections; as of January 2022, 17,500 cases have been reported in the region, a 400% increase over the 2021 incidence [1].
Despite the availability of measles vaccinations in the state and private health sectors, Namibia continues to report outbreaks of measles. The World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) estimate a national immunisation coverage of above 90% for the first dose and above 50% for the second dose from 2020 to 2023 [2]. There has been an increasing number of measles cases in the last five years, involving 10 of the 14 regions in Namibia. A total of 75 cases were reported in the Namibia measles and rubella line list, and the Erongo region reported the highest number of cases, followed by Kavango West and Ohangwena regions. Kharas, Zambezi, Hardap, and Kunene reported zero cases in the past five years. Among the 75 cases reported, five were reported in 2020, one in 2021, 20 in 2022, 25 in 2023, and 24 in 2024. Among the 75 reported cases, 18 (24%) were part of outbreaks, and the rest were sporadic. The rising burden of measles infections poses public health challenges, putting pressure on the healthcare system through the high demand for isolation facilities, inpatient care, and clinical personnel. It disrupts routine health service delivery as resources are reallocated and shifted towards outbreak containment.
The Ministry of Health and Social Services (MoHSS) manages measles cases in Namibia. The MoHSS follows the Integrated Disease Surveillance and Response (IDSR) guidelines to detect, monitor, and trace measles cases. Measles cases are recorded in the National Measles and Rubella Microsoft Access database. The database recorded 10,243 cases between January 2011 and April 2024. The cases are detected at the facilities and reported to the district and region, which report to the national level.
There is a National Expanded Programme on Immunisation (EPI) with scheduled measles vaccinations at 9 months for the first dose and 15 months for the second dose. The EPI program is free and accessible in public facilities and is paid for in the private sector [3]. Measles and rubella (MR) vaccines are administered to eligible individuals through subcutaneous injection in the upper arm [3]. The EPI provides daily immunisation services at hospitals, clinics, health centres, outreach sites, and during periodic supplementary immunisation activities (SIA) at fixed post sites and by mobile teams [3]. Approximately seven Supplementary Immunisation Activities (SIA) were carried out in Namibia from 2000 to 2023, the latest being in 2022 [3]. The coverage rates ranged from 80% to100% for the first dose and above 50% for the second dose for the past five years [3]. First-dose coverage remained consistently high between 90-91% from 2020 to 2022 [3]. There was a decline in second-dose coverage in 2021 (56.36%) compared to 2020 (63.7%) and 2022, and in 2023, second-dose coverage significantly improved to 79% [3]. Most regions peaked in 2021 and 2022, especially Oshikoto (216% in 2022) and Kavango West (155% in 2022) [4]. A general decline was observed across most regions in 2023 and 2024 [4]. Khomas consistently had the lowest vaccination coverage over the five years [4].
Despite these efforts towards measles elimination, Namibia continues to report measles outbreaks. Therefore, it is important to identify cases and understand their epidemiology so that targeted preventive measures can be implemented to successfully eliminate the virus from the population. The study describes the epidemiology of measles infections in Namibia from 2020 to 2024.
Methods
Study design and setting
This retrospective secondary data analysis study utilized the National Measles and Rubella line list from Namibia between January 2020 and April 2024. The analysis was conducted using data from all 14 regions in Namibia. Namibia has a population of 3,022,401 [5], and the majority of Namibia’s health system operates as a two-tier system comprising public and private sectors. The public health system includes 1,150 outreach points, 309 health centres, 31 districts, four intermediate/referral hospitals, and one national referral hospital [6]. There are four main seasons in Namibia, namely winter, summer, autumn, and spring. Summer starts from October to February (hot and dry), autumn starts from March to April (cooler temperatures start), winter starts from May to July (dry and cold), and spring starts from August to October (temperatures rise)
Data source and variables of interest
This study analysed measles cases extracted from the National Measles and Rubella Line List. Data were obtained from the Epidemiology Division and Expanded Programme on Immunisation with the permission of the Ministry of Health and Social Services (MoHSS) Ethics Committee. Variables such as reporting health facility, year of reporting, vaccination status, number of doses, age in years, sex, date of onset, final classification, and reporting region were used for the analysis.
Study population and sample size
This study analyzed all laboratory-confirmed IgM-positive cases and epidemiologically linked cases recorded in the measles database in Namibia from January 2020 to April 2024. The total number of positive cases reported in the line list from 2020 to 2024 was 75 (8 epidemiologically linked and 67 laboratory-confirmed). All cases that met the criteria (IgM positive and epidemiologically linked) were included.
The following standard case definitions were used in this study
Suspected case: “Any person with fever and maculopapular (non-vesicular) generalised rash and cough, coryza or conjunctivitis (red eyes) or any person in whom a clinician suspects Measles” [7].
Confirmed case: “A suspected case with laboratory confirmation (positive IgM antibody) in an outbreak” [7].
Epidemiologically linked case: “A clinical case of measles that has not been confirmed by a laboratory but was geographically and temporally related with dates of rash onset, occurring 7-21 days apart from a laboratory confirmed case or another epidemiologically linked case” [7].
Data management and analysis
Data were extracted from the National Measles and Rubella Database (line list). The line list was cleaned by removing duplicates and standardising the dates using Microsoft Excel. Unknown vaccination status was categorised separately and analysed descriptively to show the proportion of cases with unknown vaccination status. No imputation was performed for missing data. Data analysis was conducted using the Statistical Package for Social Sciences (SPSS) version 25 and Microsoft Excel to generate frequencies, proportions, and graphs, whereas Datawrapper was employed to create maps.
All IgM-positive and epidemiologically linked cases were included in this analysis. All suspected cases with negative, pending, or incompatible results were excluded from the study. Measures of central tendency (median) and dispersion (interquartile range, IQR) were used to summarise continuous variables such as age. Categorical variables, such as sex, region, vaccination status, and case classification, were summarised using frequency and proportion. The incidence rates were calculated according to region, year, and age group. Regional incidence rates were mapped to visualise geographical distribution. Age-specific incidence rates were calculated to determine the most affected group. Trends were visualised using line graphs to assess seasonality by the year of the report. Tables and graphs were used to visualise demographic characteristics. To estimate these rates, the population was disaggregated by age group, year, and region of residence. We divided the number of newly reported measles cases in each stratum by the corresponding population at risk, expressed per 100,000. Population estimates were obtained from the 2023 National Housing and Population Census.
Ethical considerations
This study adhered to the ethical guidelines outlined in the Council for International Organisations of Medical Sciences (CIOMS) guidelines, which address the use of routinely collected data for research purposes. The Research Ethics Committee of the Ministry of Health and Social Services granted approval to conduct the study. Codes instead of names were used to ensure anonymity, and no unauthorised access to the data was allowed to ensure confidentiality. Data security measures, such as locking folders on laptops, were used to protect against unauthorised access, data breaches, patient name leaks, or misuse that could harm the participants. This study did not involve direct interaction with patients; therefore, consent was not required.
Results
A total of 75 cases were analysed, of which 43 (57%) were male. The median age of the patients was 5 (Interquartile range: 2.5-9.0) years. The age group of 0-4 years had the highest representation of cases (50.1%), followed by the age group of 5-9 years (37.3%). Most patients (60%) were from rural areas (Table 1).
Among the 75 reported cases, 44% were vaccinated, with 24% of these having received the second dose and 20 % received the first dose. (Table 1). Vaccination status varied across age groups. Among children aged 0–4 years, half (50.0%) were vaccinated, while nearly one-third (31.6%) had an unknown vaccination status. In the 5–9-year age group, less than half (39.3%) were vaccinated, and half of the cases (50.0%) had unknown vaccination status. For older children aged 10–14 years, only one-quarter (25.0%) were vaccinated, with half (50.0%) having unknown vaccination status. Among adolescents aged 15–19 years, vaccination coverage was higher (50.0%), though one-quarter (25.0%) remained unvaccinated, and another quarter had an unknown status. The single case aged 20 years and above had an unknown vaccination status (Table 2).
Males generally had higher incidence rates, peaking in 2020 (2.9/100,000 population) than females (2.10/100,000) in 2020. Highest rates were observed among 0–4-year-olds from 2021 to 2023 peaking in 2023 (3.61/100,000) followed by a shift towards the 5–9-year age group in 2024 (3.16/100,000). The age group of 10-14 years generally had low incidence rates, with minor spikes in 2022 (0.31/100,000 population) and 2024 (0.92/100,000 population). The measles incidence rates for persons aged ≥ 20 years remained low (0.01/100,000) during the study period (Table 3).
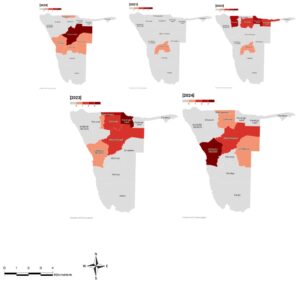
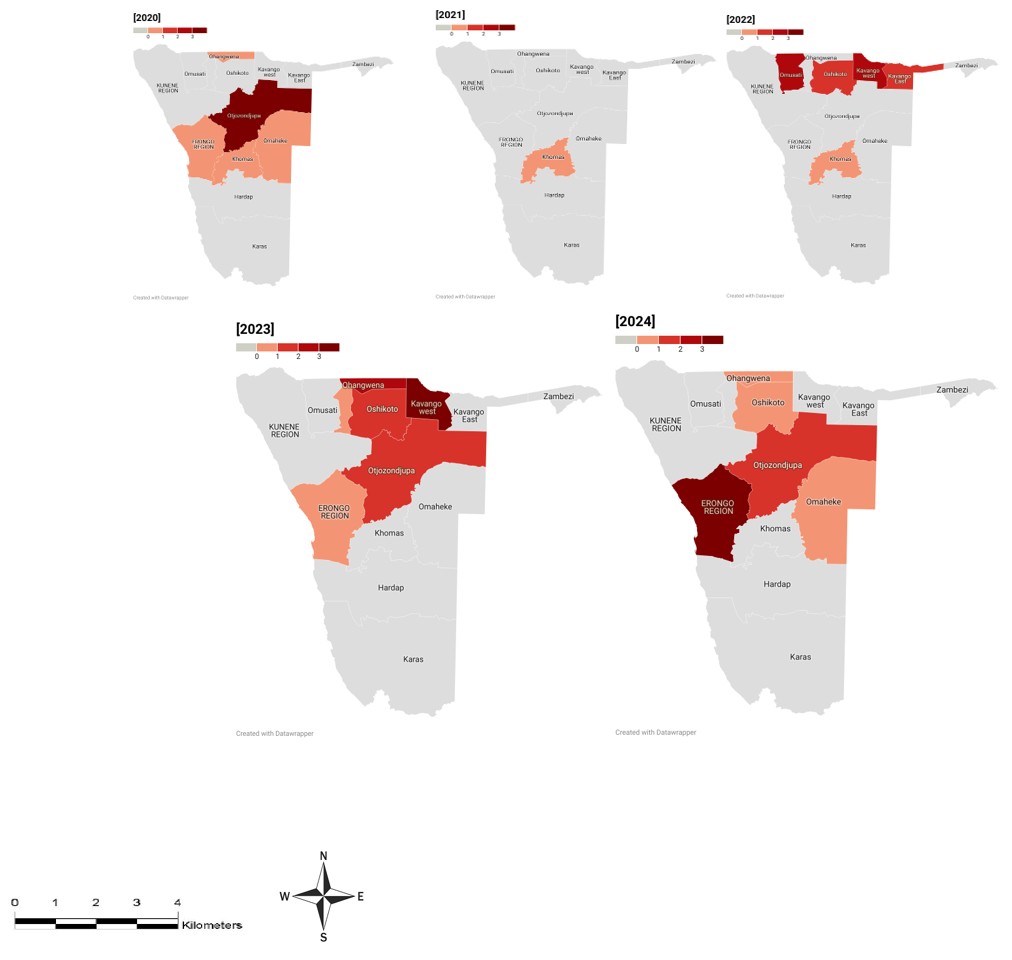
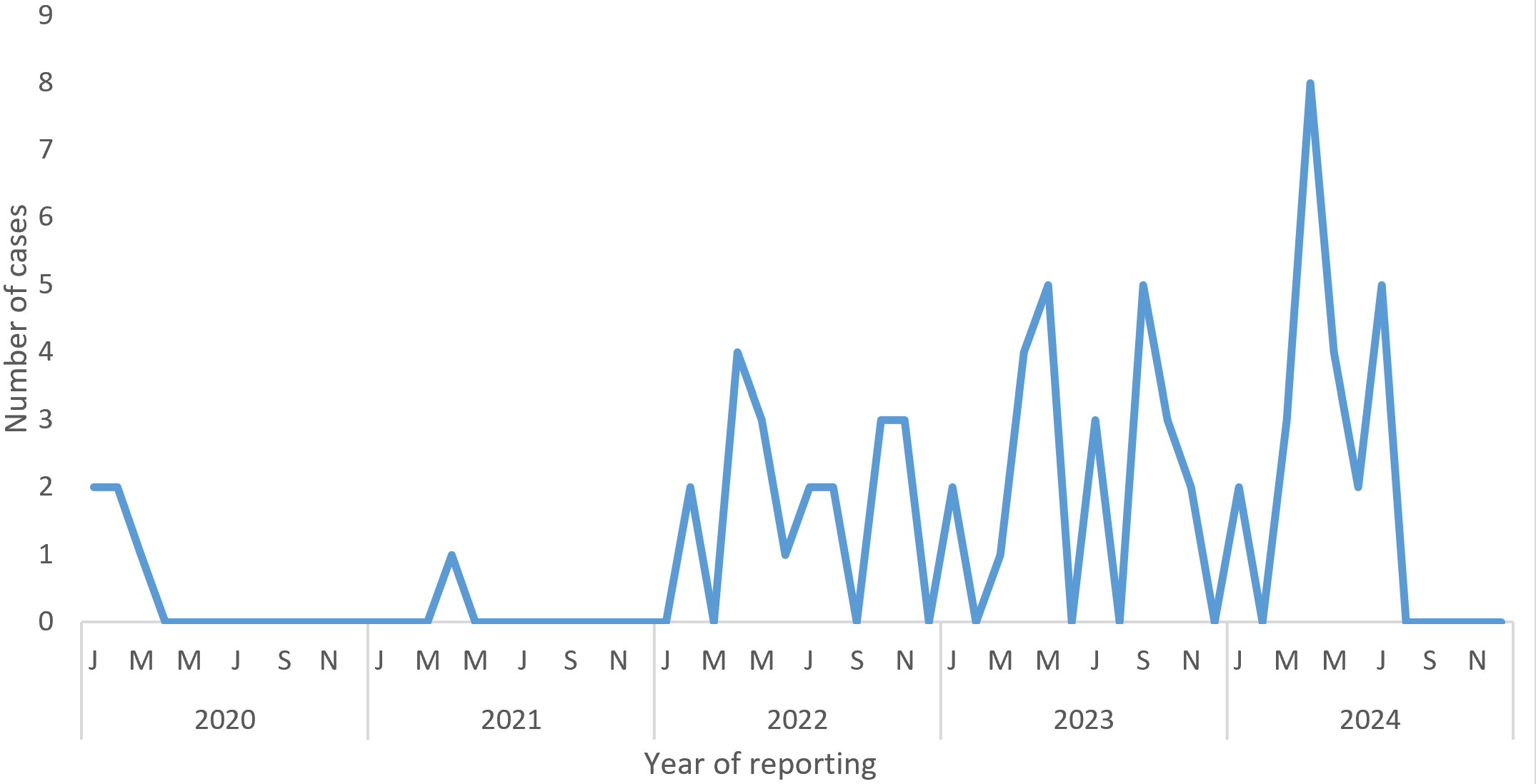
The coastal region of Erongo reported the highest regional incidence rate of 6.24 cases/100,000 population in 2024, with fluctuations over time ranging from 0.83 cases/100,000 population in 2020 to no cases in 2021 and 2022 and a re-emergence in 2023 (0.83/100,000 population). The incidence rate varied between regions, with Kavango West (2.43/100,000 in 2022 to 4.06/100,000 in 2023) and Ohangwena region (0.59/100,000 in 2020 to 2.66/100,000 in 2023), observing an increase over time, while Otjozondjupa region (3.17/100,000 in 2020 to 1.81/100,000 in 2024) had a decreasing trend. Other regions, namely, Khomas, Omaheke, Omusati, Oshana and Kavango East had fluctuating incidence rates ranging from 0.29-2.66/100,000, while Kunene, Zambezi, Hardap, and Karas had no reported cases throughout the five years (Figure 1).
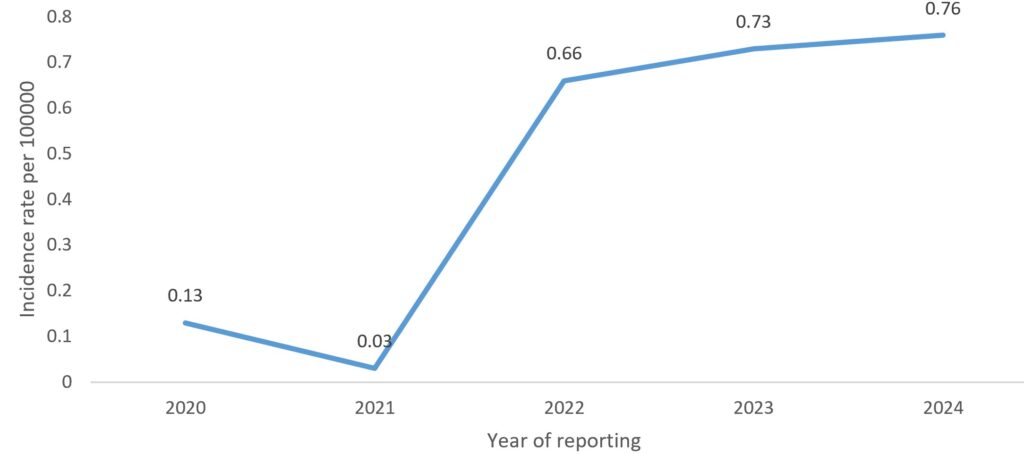
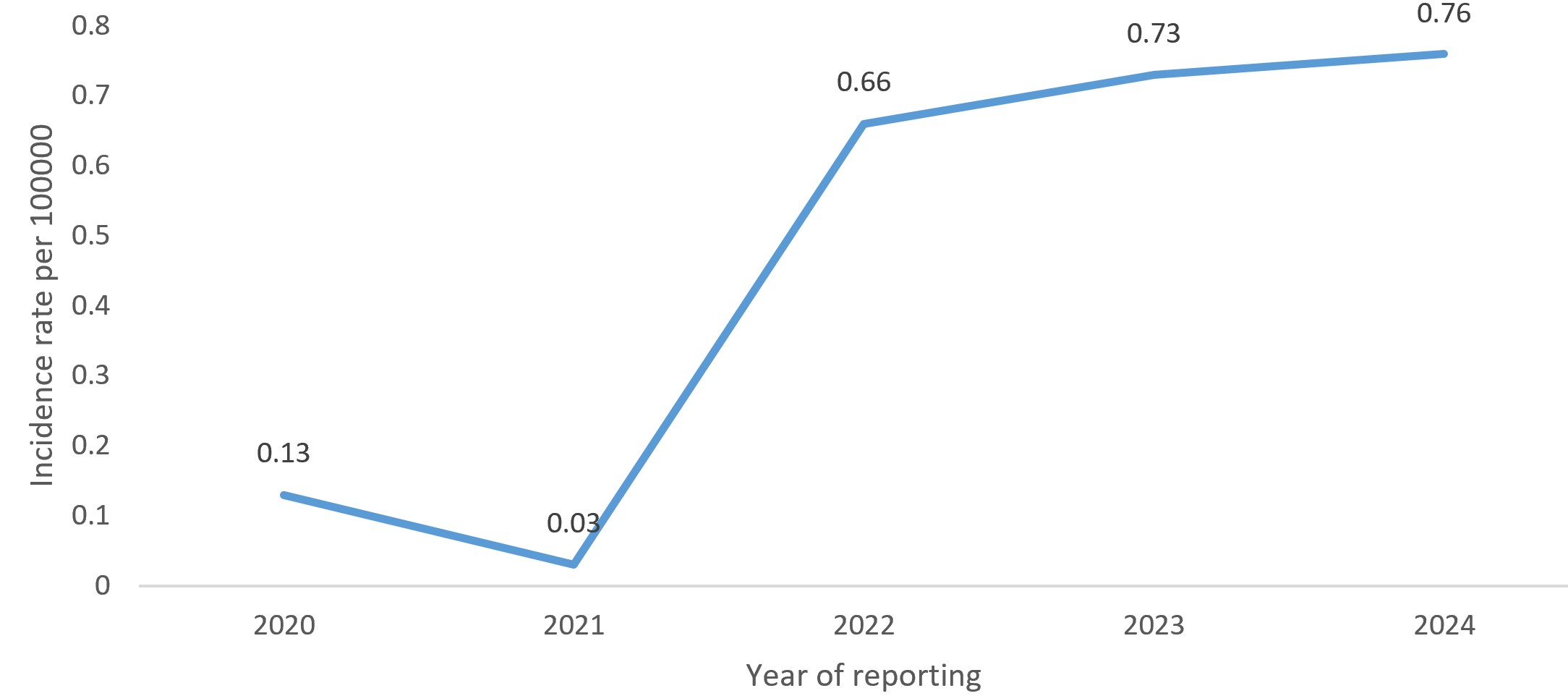
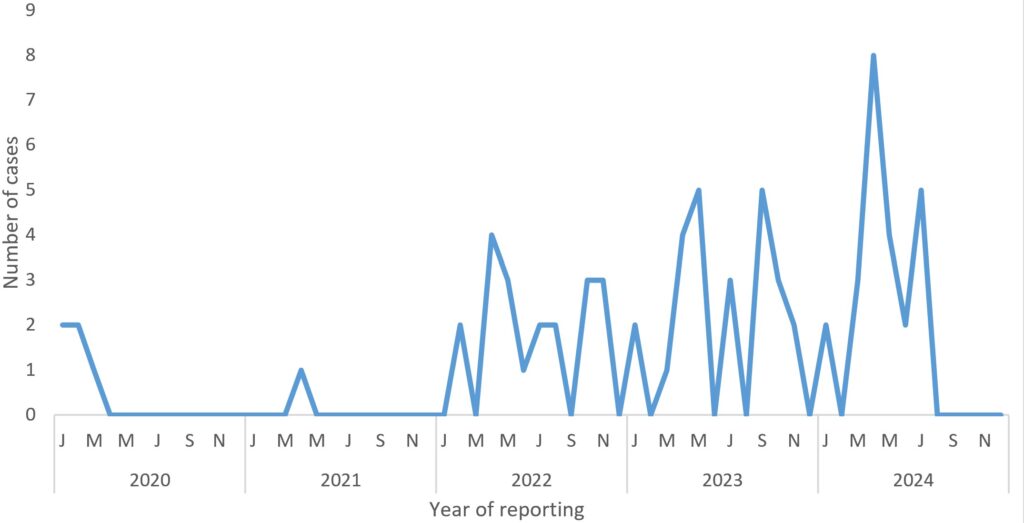
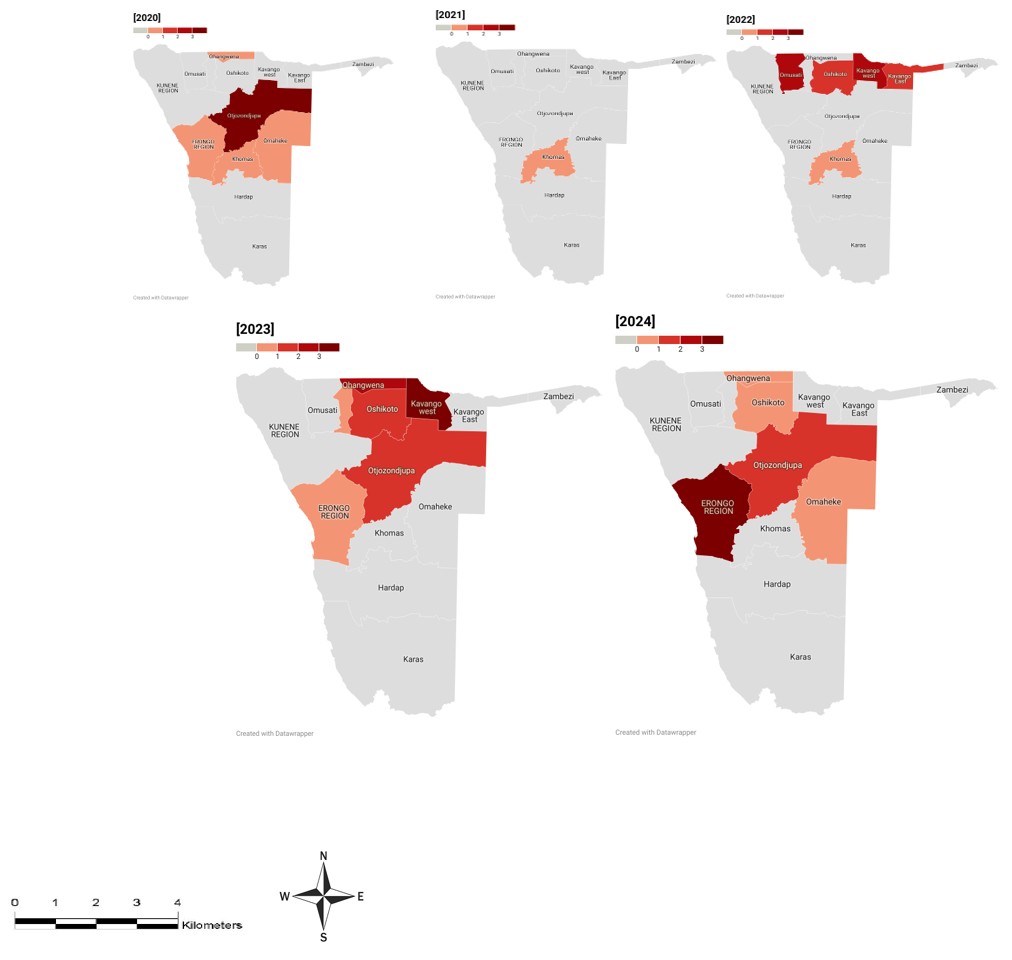
There was an overall increase in measles cases during the study period, with an initial five cases in 2020 (0.13 cases/100,000 population) to 24 cases (0.73 cases/100,000 population) in 2024. The lowest incidence was reported in 2021 (0.03 cases/100,000 population) (Figure 2). Overall, a seasonal trend was observed during the reporting period, with cases increasing annually in the winter months of April to July (Figure 3).
Discussion
Similar to other Sub-Saharan African countries, Namibia continues to report high measles incidence, particularly in children aged 0-4 years and lower incidence among those above five years [8,9]. Despite a well-established EPI programme at public health facilities nationwide and robust case-based surveillance [3], measles vaccination coverage for second dose ranged from 56 % to 79% from 2020 to 2024, well below the national target of 95% [2], driving an increase in new measles cases in Namibia. The increase in measles incidence in Namibia is likely attributable to suboptimal coverage of the second dose of the measles-containing vaccine (MCV2). The 2023 report on progress toward measles elimination in the WHO African Region showed that no country has achieved the ≥95% coverage required for herd immunity and elimination [10]. Strengthening routine and supplementary immunization activities, and enhancing surveillance are therefore essential strategies for reducing measles incidence and advancing Namibia’s progress toward elimination.
The coastal region of Erongo and the northern regions neighbouring Angola (Ohangwena and Kavango West) reported a higher measles incidence. This could be explained by the persistent burden of measles in Angola and the porous border situation between Namibia and Angola which allows increased cross-border mobility. A study conducted to evaluate the epidemiology of measles in Angola reported that measles remains a significant public health concern in Angola, with a considerable proportion occurring among the unvaccinated individuals across different provinces [11]. A recent epidemiological study conducted using routine surveillance data in Angola reported measles vaccination rates of 65% for the first dose and 40% for the second dose [11]. Findings from Sierra Leone substantiate that cross-border mobility contributes to high measles incidence, accounting for 38.1% of measles cases [12]. This highlights the need for enhanced cross-border collaboration in disease surveillance and vaccination. Strengthening coordination between Namibia and Angola through synchronised immunisation activities, data sharing, and border health checks could help reduce the importation and spread of measles cases. In addition, the persistence of measles cases in the coastal region of Erongo is in line with a study which suggested that regions in coastal settings experience prolonged outbreaks due to virus survival in cool and low-humidity settings [13]. Intensifying measles control strategies, such as conducting targeted vaccination campaigns in high-risk areas and enhancing outbreak preparedness, is necessary to reverse the increasing trend in coastal and border regions.
This study found a notable increase in measles incidence in Namibia from 2022 to 2024, with a seasonal trend in the winter season when the country experienced outbreaks. These findings are supported by previous studies [14,15] that suggested that the dry winter season, characterised by lower humidity and increased indoor crowding, may contribute to higher transmission rates. The increased incidence of measles during this period could also be due to the reduced vaccination coverage observed in 2023–2024 [4]. As countries continue to move towards repairing their healthcare systems post the COVID-19 pandemic, research suggests that vaccine hesitancy from the pandemic may have lasting effects on immunisation programs for other diseases and continues to contribute to reduced vaccination coverage [16]. Therefore, health education campaigns should focus on rebuilding community trust in vaccines and addressing misconceptions regarding vaccine safety and effectiveness. In contrast, the lower number of measles cases reported in 2020 and 2021 may be a positive outcome of COVID-19 prevention measures, such as reduced crowding, social distancing, and improved hand hygiene which temporarily reduced the transmission of various infectious diseases [17]. These findings highlight the need to strengthen routine immunisation services and maintain catch-up campaigns during and after public health emergencies and strengthen preventive measures, such as health education in communities.
Limitations
The population at risk was approximated using the total regional population owing to the lack of disaggregated data. The total number of cases analysed was obtained from the national line list; thus, cases not entered in the line list were likely missed. The high proportion of cases with unknown vaccination status made it difficult to compare the vaccinated and unvaccinated groups and to determine the variables that may be associated with poor vaccination. There are very few published studies on measles in Namibia, making it difficult to compare the findings with those in local settings.
Conclusion
A high burden of measles infection was observed among children aged 0-4 years. A seasonal trend was observed between April and June (dry and winter seasons, respectively). In the past five years, there has been a steady increase in the number of cases in the country, specifically in the northern and coastal parts of Namibia. This increasing trend could be driven by the low coverage of the second dose of the measles vaccine, and the COVID-19 pandemic potentially disrupted immunisation services. Regions bordering Angola experienced higher incidence, underscoring the importance of strengthened cross-border collaboration, including coordinated vaccination campaigns, data sharing, and border health monitoring, to prevent importation and further spread of measles Without urgent strengthening of elimination strategies, Namibia faces the risk of recurrent and escalating outbreaks of the disease.
Recommendations
Based on the findings of this study, we recommend the following actions:
- The MoHSS Health Information Systems division should improve data quality and ensure data completeness on important variables such as vaccination status.
- MoHSS EPI to strengthen existing measures to ensure greater coverage of second-dose vaccination.
- More studies on measles are recommended to better understand the factors contributing to its continued transmission
Public health actions
We conducted the following actions to improve measles surveillance in Namibia:
- Standardisation of all measles line lists (national and regional) and addition of drop-downs for all variables to ensure uniformity in data entry. By the disease surveillance officers in December 2024
- Health education sessions were conducted in the community on the importance of both vaccine doses via community meetings in Engela district, Ohangwena region with Risk Communication and Community Engagement Officers.
What is already known about the topic
- Measles is at elimination stage in Namibia
- The measles outbreaks dropped after the introduction of second dose vaccination in 2016
- Children aged under 5 years are at a higher risk of contracting measles
What this study adds
- Measles incidence is observed to be higher in winter (between April and June)
- The cases are on the rise on the northern and coastal areas and sporadic country wide
- Measles cases are present in adults and among the vaccinated group
- There is low vaccination coverage for the measles second dose
Acknowledgements
The authors acknowledge the Namibia Ministry of Health and Social Services Health Information and Research Directorate, University of Namibia, Expanded Program on Immunisation, Namibia Field Epidemiology and Laboratory Training Program, and NAMFELTP colleagues for their contributions.
Data availability
The Ministry of Health and Social Services, Health Information and Research Directorate, Epidemiology Division manages the data. The data will be available upon request with ethical clearance from the authors/institution.
List of abbreviations
CIOMS: Council for International Organisations of Medical
EPI: Expanded Programme on Immunisation
COVID-19: Coronavirus Disease 2019
DHIS2: District Health Information 2
IDSR: Integrated Disease Surveillance and Response
IgM: Immunoglobulin M
IQR: Interquartile Range
MCV2: Measles-Containing Vaccine, Second Dose
MoHSS: Ministry of Health and Social Services
MR: Measles and Rubella
NAMFELTP: Namibia Field Epidemiology and Laboratory Training Program
SIA: Supplementary Immunization Activity
SPSS: Statistical Package for the Social Sciences
UNICEF: United Nations Children’s Fund
WHO: World Health Organization
Authors´ contributions
Monika Densi and Nelly Shalo Ntusi were responsible for data analysis and interpretation and manuscript development. Ndeshihafela Sakaria and Dianah Ewaga supervised the study from concept development to manuscript development and revision. Silas Nghishihange and Secilia Nghidishange, reviewed the manuscript for submission. All authors have read and approved the final manuscript.
| Characteristics | Frequency (n=75) | Percentage (%) |
|---|---|---|
| Sex | ||
| Female | 32 | 42.7 |
| Male | 43 | 57.3 |
| Place of residence | ||
| Urban | 30 | 40.0 |
| Rural | 45 | 60.0 |
| Age (years) | ||
| 0–4 | 38 | 50.7 |
| 5–9 | 28 | 37.3 |
| 10–14 | 4 | 5.3 |
| 15–19 | 4 | 5.3 |
| 20+ | 1 | 1.3 |
| Vaccination status | ||
| Not Vaccinated | 12 | 16.0 |
| Vaccinated | 33 | 44.0 |
| Unknown | 30 | 40.0 |
| Number of vaccine doses | ||
| Vaccinated 1st dose | 15 | 20.0 |
| Vaccinated 2nd dose | 18 | 24.0 |
| Not vaccinated | 12 | 16.0 |
| Unknown vaccination status | 30 | 40.0 |
| Age group | Vaccination status | Total | ||
|---|---|---|---|---|
| Vaccinated n (%) | Not vaccinated n (%) | Unknown vaccination status n (%) | ||
| 0–4 | 19 (50.0) | 7 (18.4) | 12 (31.6) | 38 |
| 5–9 | 11 (39.0) | 3 (10.7) | 14 (50.0) | 28 |
| 10–14 | 1 (25.0) | 1 (25.0) | 2 (50.0) | 4 |
| 15–19 | 2 (50.0) | 1 (25.0) | 1 (25.0) | 4 |
| 20+ | 0 (0) | 0 (0.0) | 1 (100) | 1 |
| Variable | Incidence rates 2020 | Incidence rates 2021 | Incidence rates 2022 | Incidence rates 2023 | Incidence rates 2024 |
|---|---|---|---|---|---|
| Age group | |||||
| 0–4 | 0.96 | 0.24 | 2.89 | 3.61 | 1.92 |
| 5–9 | 0.79 | 0.00 | 1.58 | 1.84 | 3.16 |
| 10–14 | 0.00 | 0.00 | 0.31 | 0.00 | 0.92 |
| 15–19 | 1.40 | 0.00 | 0.00 | 1.08 | 0.36 |
| 20+ | 0.01 | 0.06 | 0.00 | 0.00 | 0.00 |
| Gender | |||||
| Male | 2.90 | 0.27 | 0.07 | 1.15 | 0.81 |
| Female | 2.10 | 0.06 | 0.71 | 0.52 | 0.78 |
References
- Nchasi G, Paul IK, Sospeter SB, Mallya MR, Ruaichi J, Malunga J. Measles outbreak in sub-Saharan Africa amidst COVID-19: A rising concern, efforts, challenges, and future recommendations. Ann Med Surg (Lond) [Internet]. 2022 Jul 31 [cited 2026 Feb 18];81:104264. doi:10.1016/j.amsu.2022.104264. Available from: https://journals.lww.com/10.1016/j.amsu.2022.104264.
- World Health Organization (WHO). Measles vaccination coverage [Internet]. Geneva (Switzerland): World Health Organization; 2024 [cited 2026 Feb 18]. Available from: https://immunizationdata.who.int/global/wiise-detail-page/measles-vaccination-coverage?CODE=NAM&ANTIGEN=MCV1&YEAR=.
- Masresha BG, Shibeshi ME, De Wee R, Shapumba N, Sayi T, Reef SE, Goodson JL. On the Path to Measles and Rubella Elimination Following Rubella-Containing Vaccine Introduction, 2000–2023, Namibia. Vaccines (Basel) [Internet]. 2024 Aug 23 [cited 2026 Feb 18];12(9):957. doi:10.3390/vaccines12090957. Available from: https://www.mdpi.com/2076-393X/12/9/957.
- Ministry of Health and Social Services (Namibia). District Health Information Systems [Internet]. Windhoek (Namibia): Ministry of Health and Social Services; 2025 [cited 2026 Feb 18]. Available from: https://hmis.mhss.gov.na (Subscription required to access full text).
- Namibia Statistics Agency. Namibia 2023 Population and Housing Census: Main report [Internet]. Windhoek (Namibia): Namibia Statistics Agency; 2024 [cited 2026 Feb 18]. 93 p. Available from: https://nsa.org.na/census/wp-content/uploads/2024/10/2023-Population-and-Housing-Census-Main-Report-28-Oct-2024.pdf.
- Ministry of Health and Social Services (Namibia). Services [Internet]. Windhoek (Namibia): Ministry of Health and Social Services; [cited 2026 Feb 18]. Available from: https://mhss.gov.na/services.
- Ministry of Health and Social Services (Namibia), World Health Organization (Namibia). National technical guidelines for disease surveillance and response: 3rd ed. Part II, March 2023 [Internet]. Windhoek (Namibia): Ministry of Health and Social Services (Namibia), World Health Organization (Namibia); 2023 Oct [cited 2026 Feb 18]. 199 p. Available from: https://mhss.gov.na/documents/-/document_library/mqih/view_file/6988359.
- Ori PU, Adebowale A, Umeokonkwo CD, Osigwe U, Balogun MS. Descriptive epidemiology of measles cases in Bauchi State, 2013–2018. BMC Public Health [Internet]. 2021 Jun 5 [cited 2026 Feb 18];21(1):1311. doi:10.1186/s12889-021-11063-6. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-11063-6.
- Tefera SF, Admasu N, Abebe H, Feyisa GC, Midaksa G. Measles outbreak investigation in Tocha district, southwestern Ethiopia: an unmatched case–control study. Front Public Health [Internet]. 2024 Apr 10 [cited 2026 Feb 18];12:1331798. doi:10.3389/fpubh.2024.1331798. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1331798/full.
- Masresha BG, Hatcher C, Lebo E, Tanifum P, Bwaka AM, Minta AA, Antoni S, Grant GB, Perry RT, O’Connor P. Progress Toward Measles Elimination — African Region, 2017–2021. MMWR Morb Mortal Wkly Rep [Internet]. 2023 Sep 8 [cited 2026 Feb 18];72(36):985–91. doi:10.15585/mmwr.mm7236a3. Available from: http://www.cdc.gov/mmwr/volumes/72/wr/mm7236a3.htm?s_cid=mm7236a3_w.
- Ramírez MA, Fernádez Santisteban MT, Galange MM, Carralero RR, Júlio G, Samutondo C, Gaston C, Manuel E, Pedro AM, Paixão J, Freitas H, Morais J, Francisco NM. Epidemiology of measles in Angola: Results from routine surveillance from 2015 to 2021. IJID Reg [Internet]. 2023 Apr 9 [cited 2026 Feb 18];7:256–61. doi:10.1016/j.ijregi.2023.04.004. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2772707623000462.
- Bah MS, Elduma AH, Sesay U, Hakizimana JL, Gebru GN, Menyenyere H, Kallon B. Factors associated with measles infection in border and non-border districts of Sierra Leone. Sierra Leone J Biomed Res [Internet]. 2024 Oct [cited 2026 Feb 18];15(1):37–49. doi:10.4314/sljbr.v15i1.7. Available from: https://www.sljbr.org/index.php/sjbmr/article/view/213.
- Bharti N, Xia Y, Bjornstad ON, Grenfell BT. Measles on the Edge: Coastal Heterogeneities and Infection Dynamics. PLoS ONE [Internet]. 2008 Apr 9 [cited 2026 Feb 18];3(4):e1941. doi:10.1371/journal.pone.0001941. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0001941.
- Wudu H, Alemu C, Minalu W, Berelie H, Bantie D. Trend and forecast of measles disease, in East Gojjam Zone, Amhara Region, Northwest Ethiopia, 2023: A cross-sectional study. BMC Res Notes [Internet]. 2024 Dec 24 [cited 2026 Feb 18];17(1):383. doi:10.1186/s13104-024-07057-3. Available from: https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-024-07057-3.
- Shobayo B, Umeokonkwo CD, Jetoh RW, Gilayeneh JSM, Akpan G, Amo-Addae M, Macauley J, Idowu RT. Descriptive Analysis of Measles Outbreak in Liberia, 2022. IJID Reg [Internet]. 2024 Jan 26 [cited 2026 Feb 18];10:200–6. doi:10.1016/j.ijregi.2024.01.008. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2772707624000092.
- Niikondo A, Awofolu O. Effectiveness and impact of COVID-19 response and vaccination challenges in Namibia: a systematic review. J Public Health Afr [Internet]. 2023 Dec 30 [cited 2026 Feb 18];14(12):27. doi:10.4081/jphia.2024.2094. Available from: https://publichealthinafrica.org/index.php/jphia/article/view/10.
- Farid M, Fahmy K, Ghoniem A, Sharifuzzaman M, Hasan Q, Crowcroft N, O’Connor P. Progress of Measles and Rubella Surveillance in the Context of Measles Elimination in the WHO Eastern Mediterranean Region, 2019–2022. Vaccines (Basel) [Internet]. 2024 Nov 29 [cited 2026 Feb 18];12(12):1349. doi:10.3390/vaccines12121349. Available from: https://www.mdpi.com/2076-393X/12/12/1349.
