Perspective | Open Access | Volume 8 (4): Article 81 | Published: 08 Oct 2025
Building resilience: Leveraging the integrated disease surveillance and response strategy for antimicrobial resistance surveillance in Tanzania
Menu, Tables and Figures
On Google Scholar
Navigate this article
Figures
Keywords
- Antimicrobial Resistance
- Integrated Disease Surveillance
- Response
Vulstan James Shedura1,&, Ally Kassim Hussein2, Herbert George Masigati3
1Department of Clinical Research, Training, and Consultancy, Southern Zone Referral Hospital, Mtwara, Tanzania, 2Department of Epidemiology, Tanzania Field Epidemiology and Laboratory Training Program, 3Department of General Surgery, Southern Zone Referral Hospital, Mtwara, Tanzania
&Corresponding author: Vulstan James Shedura, Department of Clinical Research, Training, and Consultancy, Southern Zone Referral Hospital, P.O. Box 272, Mtwara, Tanzania.
Email: vulstanshedura@gmail.com ORCID: https://orcid.org/0000-0002-1939-2492
Received: 26 Dec 2024, Accepted: 06 Oct 2025, Published: 08 0ct 2025
Domain: Field Epidemiology, Antimicrobial Resistance, Public Health Disease Surveillance
Keywords: Antimicrobial Resistance, Integrated Disease Surveillance, Response
©Vulstan James Shedura et al. Journal of Interventional Epidemiology and Public Health (ISSN: 2664-2824). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Vulstan James Shedura et al., Building resilience: Leveraging the integrated disease surveillance and response strategy for antimicrobial resistance surveillance in Tanzania. Journal of Interventional Epidemiology and Public Health. 2025;8(4):81. https://doi.org/10.37432/JIEPH-D-24-02069
Abstract
Antimicrobial resistance (AMR) poses an escalating threat to global public health, undermining the effectiveness of essential treatments and placing additional strain on healthcare systems, especially in low- and middle-income countries like Tanzania. While Tanzania has made progress through the establishment of laboratory-based AMR sentinel sites under a One Health framework, the current system remains limited in scale, data sharing, and coverage across healthcare levels. Integrating AMR surveillance into the existing Integrated Disease Surveillance and Response (IDSR) strategy offers a practical and scalable solution to address these gaps. The IDSR framework, established by the World Health Organization Regional Office for Africa and the U.S. Centers for Disease Control and Prevention, provides a robust platform for early detection, reporting, and coordinated response to priority health threats. This paper explores the rationale, mechanisms, and potential benefits of aligning AMR surveillance with IDSR in Tanzania, including broader data capture, improved laboratory capacity at peripheral levels via adopting the Laboratory-Hub-Spoke Model (LHSM), strengthened One Health collaboration, and real-time decision-making. Drawing on lessons from regional contexts and identifying key implementation challenges, the integration is proposed as a strategic approach to building a resilient and responsive AMR surveillance system in Tanzania and similar settings.
Perspective
Introduction
Antimicrobial resistance (AMR) is among the most significant global health threats of the 21st century. The increasing prevalence of resistant pathogens undermines the effectiveness of antibiotics, leading to prolonged illnesses, increased healthcare costs, and higher mortality rates [1, 2]. While efforts to address AMR have intensified globally, the challenge persists, particularly in low- and middle-income countries (LMICs), where health systems are often weak. Tanzania faces a growing AMR burden, worsened by irrational antimicrobial use, insufficient regulatory frameworks, and inadequate infection prevention and control (IPC) practices [3]. Against this backdrop, integrating AMR surveillance into the Integrated Disease Surveillance and Response (IDSR) strategy offers a promising avenue to monitor resistance patterns, inform policies, and strengthen antimicrobial stewardship efforts.
Globally, AMR accounted for an estimated 4.95 million deaths in 2019, with 1.27 million deaths directly attributable to resistant infections [4]. The economic implications are staggering, with projections suggesting that unchecked AMR could result in a $100 trillion loss in global output by 2050 [5]. Western sub-Saharan Africa bears the heaviest burden, with mortality rates reaching 27.3 deaths per 100,000 population [6, 7].
In Tanzania, AMR resistance rates for common pathogens range from 25% to 50%, driven by the overuse of antibiotics, self-medication, and weak healthcare systems [3]. Infections caused by multidrug-resistant (MDR) pathogens, such as Klebsiella pneumoniae and Escherichia coli, contribute significantly to the country’s healthcare-associated infections (HAIs). Despite the implementation of the National Action Plan (NAP) on AMR, gaps in surveillance, infrastructure, and cross-sectoral collaboration remain unaddressed.
The IDSR strategy, introduced in the late 1990s, aims to enhance disease surveillance and response through a unified framework that connects community, health facility, district, regional, and national levels [2]. By adopting a One Health perspective, the strategy integrates human, animal, and environmental health components, addressing emerging and re-emerging threats. Incorporating AMR surveillance into the IDSR framework can facilitate real-time monitoring, improve outbreak responses, and promote evidence-based policymaking.
Rationale for Integrating AMR Surveillance into IDSR
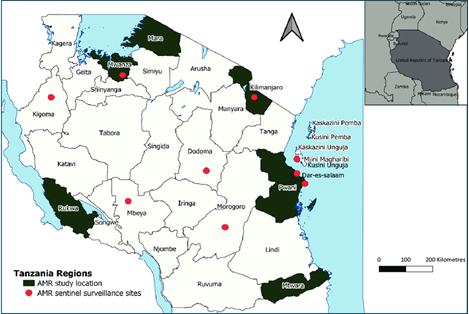
The integration of AMR surveillance into Tanzania’s IDSR framework is a strategic necessity in light of the escalating resistance crisis and the limitations of the current surveillance system [3]. Although Tanzania has made commendable progress through the establishment of nine sentinel AMR surveillance sites under the One Health framework (Figure 1), the system remains laboratory-based and limited to a few tertiary-level facilities [8]. This restricts geographic coverage and delays the detection of resistance trends in peripheral and community settings. Moreover, the sharing of surveillance data across human, animal, and environmental health sectors remains fragmented, undermining coordinated national responses [8, 9].
The current laboratory-based surveillance system is further challenged by inadequate laboratory infrastructure, particularly at primary and secondary levels [8]. Most of the lower-tier health facilities are unable to perform culture and antimicrobial susceptibility testing (AST) due to a lack of equipment, trained personnel, and standardised procedures [8, 10]. The absence of local antibiograms also leads to empirical and often inappropriate antibiotic prescribing, fueling further resistance. These gaps suggest that while the existing system is foundational, it is insufficient for comprehensive AMR surveillance, especially at the community level [8, 9].
Integrating AMR surveillance into the IDSR system offers a practical and scalable solution to address these limitations. Unlike the sentinel-based system, IDSR is implemented across all healthcare levels in Tanzania and has a well-established mechanism for weekly disease reporting via mobile technology and digital platforms [8]. By designating AMR as a weekly reportable condition and enabling culture and AST at more decentralized levels, IDSR can facilitate early detection, timely reporting, and rapid response to resistance threats. Importantly, IDSR’s structured processes, including case detection, notification, verification, and feedback, can enhance the use of AMR data for action at all levels of the health system.
Ghana’s experience further reinforces the feasibility of this integration. By incorporating laboratory-based AMR data into its IDSR framework, Ghana has strengthened early warning systems and facilitated prompt public health responses to resistant infections [1, 11, 12]. Similarly, regional assessments from Zambia and East Africa reveal that while laboratory-based AMR surveillance is often poorly resourced, IDSR-like structures hold promise for expanding reach and enabling real-time data flows [9, 10].
Integrating AMR surveillance into the IDSR framework represents a cost-effective, system-wide approach to overcoming the limitations of Tanzania’s current lab-based AMR system. It has the potential to expand surveillance coverage, strengthen One Health collaboration, and support timely, evidence-based interventions for AMR containment.
Mechanisms for Leveraging AMR Surveillance in the IDSR Framework
The IDSR framework utilizes both Indicator-Based Surveillance (IBS) and Event-Based Surveillance (EBS) to capture structured and unstructured public health data across Tanzania [2]. While AMR surveillance in the country is currently guided by a laboratory-based model aligned with the One Health framework, it remains limited in scale, primarily implemented in only nine established sentinel sites, and largely restricted to secondary and tertiary-level hospitals [8]. Integration of AMR surveillance into the IDSR system could offer a broader, more systematic platform for detection, notification, and response by leveraging the extensive health facility network through which IDSR operates.
A key integration mechanism is to decentralize culture and AST by (i) investing in basic microbiology capacity at primary and secondary facilities, including essential equipment, quality control (QC) materials, and staff upskilling, and (ii) leveraging a Laboratory-Hub-and-Spoke Model (LHSM) in which peripheral “spokes” handle specimen collection and selected tests, while regional/tertiary “hubs” provide confirmatory testing, mentorship, e-learning, antibiogram development, and data management. This dual approach addresses current gaps, including limited local antibiograms, inadequate equipment, and peripheral staffing shortages, while ensuring standardized methods and rapid escalation pathways. AMR results from both spokes and hubs will flow into routine IDSR reporting and GLASS-aligned dashboards to guide empirical therapy and policy. Evidence from Tanzania’s surveillance experience and Ghana’s IDSR-based AMR implementation demonstrates feasibility [8, 10]. Evidence from Sub-Saharan Africa demonstrates that this approach enhances feasibility by strengthening diagnostic capacity, improving antimicrobial stewardship (AMS) implementation, and optimising resource utilization in resource-limited settings [13]. The LHSM’s structure promotes decentralization of culture and AST services, facilitates standardized data reporting into IDSR and GLASS platforms, and supports scalability through phased expansion from sentinel spokes [13].
The integration process can be operationalised through the inclusion of AMR as a weekly reportable condition under the IDSR system. This would enable early case identification and data transmission using mobile technologies already embedded in IDSR reporting channels [11]. Furthermore, the adoption of digital tools, such as the Surveillance Outbreak Response Management and Analysis System (SORMAS), and the incorporation of AMR indicators can enhance real-time data sharing and analysis. Artificial intelligence-driven analytics could support the identification of resistance trends and inform outbreak response and antimicrobial stewardship [9, 11].
Moreover, integration into IDSR supports the principles of the One Health approach by fostering collaboration among the human, animal, and environmental health sectors. However, evidence from across the region shows that the animal and environmental sectors often have minimal capacity for AMR surveillance [9]. By using IDSR’s structured systems and promoting cross-sectoral engagement, integration could catalyze unified surveillance efforts and coordinated responses.
The AMR-IDSR integration should be viewed not as a replacement of the current lab-based sentinel surveillance system but as a complementary strategy to expand reach, streamline data collection, and strengthen early warning systems for resistant infections.
Potential Challenges and Mitigation Strategies for AMR–IDSR Integration
Integration of AMR surveillance into the IDSR framework in Tanzania is not without challenges. First, there is insufficient laboratory capacity at lower-level facilities to perform culture and AST technologies that are essential for reliable AMR detection. The absence of local antibiograms and limited access to quality-controlled diagnostic reagents worsen irrational antimicrobial use, causing resistance. Secondly, there is a human resource gap. Many healthcare workers, particularly at the primary care level, are not trained in AMR diagnostics, reporting procedures, or antimicrobial stewardship. This could significantly undermine data quality and timeliness. Third, weak intersectoral data sharing between human, veterinary, and environmental health sectors limits the realization of a truly One Health-oriented surveillance system.
To mitigate these challenges, a phased implementation approach can be adopted. This includes: (i) upgrading laboratories with capacity for culture and AST, starting with high-burden regions; (ii) adopting LHSM by creating sub-national AMR coordination units within each “hub” to provide continuous mentorship, supervision, and quality assurance to “spoke” laboratories, thereby ensuring consistency and sustainability of LHSM operations; (iii) incorporating AMR training into IDSR cascade training modules; (iv) using digital health tools like electronic IDSR and SORMAS to streamline reporting; and (v) promoting data-sharing protocols across sectors to support collaborative interventions.
Way Forward and Recommendations
To effectively integrate AMR surveillance into Tanzania’s IDSR framework, a comprehensive, coordinated, and sustainable strategy is required. This should prioritize strengthening laboratory capacity at primary and secondary health facilities to enable culture and AST, complemented by the adoption of LHSM. Under this model, well-equipped regional or tertiary laboratories (“hubs”) provide confirmatory testing, mentorship, and data management support to peripheral health facilities (“spokes”), enhancing diagnostic capacity and ensuring standardized AMR data flow into IDSR and GLASS systems. Institutionalizing continuous professional development programs for healthcare workers in AMR diagnostics, surveillance, and IPC will be critical. The government should further integrate AMR as a formal notifiable condition within the IDSR system and allocate sustainable domestic funding for infrastructure, human resources, and operational activities. Leveraging digital surveillance tools such as SORMAS and mobile IDSR platforms can enhance real-time reporting and linkage of AMR data across the health system. Cross-sectoral collaboration under the One Health approach should be reinforced through strong data-sharing protocols connecting human, animal, and environmental health sectors. Public awareness campaigns are also essential to promote responsible antibiotic use and community participation in AMR prevention. Importantly, leveraging the existing IDSR platform to accommodate AMR surveillance serves as a strategic mitigation measure amid declining international support, including reductions in funding from the US government and the UK’s Fleming Fund, which have historically supported public health laboratories across Africa [9, 14]. Strengthening and optimizing Tanzania’s existing surveillance infrastructure, therefore, makes both economic and operational sense, ensuring long-term sustainability and national ownership of AMR monitoring. Finally, a strong monitoring and evaluation system with clear indicators should be established to track progress, ensure accountability, and inform continuous improvement of AMR-IDSR integration.
Conclusion
The integration of antimicrobial resistance surveillance into Tanzania’s IDSR framework presents a strategic and scalable opportunity to strengthen the country’s capacity to detect, monitor, and respond to AMR threats. Although Tanzania has made notable progress in establishing sentinel sites under the One Health framework, these efforts remain limited in coverage, and data sharing between sectors remains weak. Integration into the IDSR can address existing gaps by leveraging its expansive network, digital infrastructure, and reporting mechanisms. However, successful integration demands sustained investment, cross-sectoral collaboration, and deliberate strategies to overcome infrastructure and human resource barriers. The use of the LHSM in AMR surveillance is an effective strategy for strengthening diagnostic capacity and ensuring the generation of accurate and reliable data. This model has also proven successful in other disease programs, such as HIV, TB, polio, and measles, through the use of integrated sample referral systems [15, 16]. By addressing these limitations and committing to long-term action, Tanzania can position itself as a regional leader in AMR surveillance and contribute meaningfully to the global fight against antimicrobial resistance.
Call to Action: Policymakers, public health leaders, and development partners should prioritize the integration of AMR surveillance into the IDSR framework, recognizing it as essential for the sustainability and effectiveness of Tanzania’s disease surveillance architecture and for safeguarding future treatment options.
References
- World Health Organization. One Health Approach for Global Health Security [Internet]. Geneva (Switzerland): World Health Organization; 2020 [cited 2024 Dec 23]. Available from: https://www.who.int/health-topics/one-health#tab=tab_1.
- World Health Organization. Technical Guidelines for Integrated Disease Surveillance and Response in the African Region: Third edition [Internet]. Brazzaville (Republic of the Congo): WHO Regional Office for Africa; 2019 [cited 2024 Dec 23]. Available from: https://www.afro.who.int/publications/technical-guidelines-integrated-disease-surveillance-and-response-african-region-third.
- Kumburu HH, Sonda T, van Zwetselaar M, Leekitcharoenphon P, Lukjancenko O, Mmbaga BT, Alifrangis M, Lund O, Aarestrup FM, Kibiki GS. Using WGS to identify antibiotic resistance genes and predict antimicrobial resistance phenotypes in MDR Acinetobacter baumannii in Tanzania. J Antimicrob Chemother [Internet]. 2019 Jun 1 [cited 2025 Oct 7];74(6):1484-93. Available from: https://academic.oup.com/jac/article/74/6/1484/5370329. doi: 10.1093/jac/dkz055.
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet [Internet]. 2022 Feb 12 [cited 2025 Oct 10];399(10325):629-55. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)02724-0/fulltext. doi: 10.1016/S0140-6736(21)02724-0.
- Price R. O’Neill report on antimicrobial resistance: funding for antimicrobial specialists should be improved. Eur J Hosp Pharm [Internet]. 2016 Jul [cited 2025 Oct 7];23(4):245-7. Available from: https://ejhp.bmj.com/lookup/doi/10.1136/ejhpharm-2016-001013. doi: 10.1136/ejhpharm-2016-001013.
- World Health Organization. Global action plan on antimicrobial resistance [Internet]. Geneva (Switzerland): World Health Organization; 2019 Jan 1 [cited 2024 Dec 23]. Available from: https://www.who.int/publications/i/item/9789241509763.
- Okeke IN, de Kraker MEA, van Boeckel TP, Kumar CK, Schmitt H, Gales AC, Bertagnolio S, Sharland M, Laxminarayan R. The scope of the antimicrobial resistance challenge. Lancet [Internet]. 2024 Jun 8 [cited 2025 Oct 7];403(10442):2426-38. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673624008766. doi: 10.1016/S0140-6736(24)00876-6.
- Camara N, Moremi N, Mghamba J, Eliakimu E, Shumba E, Ondoa P, Egyir B. Surveillance of antimicrobial resistance in human health in Tanzania: 2016–2021. Afr J Lab Med [Internet]. 2023 May 22 [cited 2025 Oct 7];12(1):e2053. Available from: https://ajlmonline.org/index.php/ajlm/article/view/2053. doi: 10.4102/ajlm.v12i1.2053.
- Matee M, Mshana SE, Mtebe M, Komba EV, Moremi N, Lutamwa J, Kapona O, Sekamatte M, Mboera LEG. Mapping and gap analysis on antimicrobial resistance surveillance systems in Kenya, Tanzania, Uganda and Zambia. Bull Natl Res Cent [Internet]. 2023 Jan 30 [cited 2025 Oct 7];47(1):12. Available from: https://bnrc.springeropen.com/articles/10.1186/s42269-023-00986-2. doi: 10.1186/s42269-023-00986-2.
- Shempela DM, Mudenda S, Kasanga M, Daka V, Kangongwe MH, Kamayani M, Sikalima J, Yankonde B, Kasonde CB, Nakazwe R, Mwandila A, Cham F, Njuguna M, Simwaka B, Morrison L, Chizimu JY, Muma JB, Chilengi R, Sichinga K. A situation analysis of the capacity of laboratories in faith-based hospitals in Zambia to conduct surveillance of antimicrobial resistance: opportunities to improve diagnostic stewardship. Microorganisms [Internet]. 2024 Aug 17 [cited 2025 Oct 7];12(8):1697. Available from: https://www.mdpi.com/2076-2607/12/8/1697. doi: 10.3390/microorganisms12081697.
- Egyir B, Bortey A, Duedu KO, Boateng G, Bekoe FA, Hedidor G, Adjabeng M, Dayie NTKD, Obeng-Nkrumah N, Opintan JA. Implementation of antimicrobial resistance surveillance in Ghana using the Integrated Disease Surveillance and Response strategy. Afr J Lab Med [Internet]. 2024 Aug 13 [cited 2025 Oct 7];13(1):e2404. Available from: https://ajlmonline.org/index.php/ajlm/article/view/2404. doi: 10.4102/ajlm.v13i1.2404.
- Turner P, Fox-Lewis A, Shrestha P, Dance DAB, Wangrangsimakul T, Cusack TP, Ling CL, Hopkins J, Roberts T, Limmathurotsakul D, Cooper BS, Dunachie S, Dolecek C, van Doorn HR, Guerin PJ, Day NPJ, Ashley EA. Microbiology Investigation Criteria for Reporting Objectively (Micro): a framework for the reporting and interpretation of clinical microbiology data. BMC Med [Internet]. 2019 Dec [cited 2025 Oct 7];17(1):70. Available from: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1301-1. doi: 10.1186/s12916-019-1301-1.
- Iqbal A, Kumaradev Y, Gülpinar G, Brandish C, Nabiryo M, Garraghan F, Rosado H, Rutter V. Application of the hub-and-spoke model in antimicrobial stewardship programmes: a scoping review. BioMed [Internet]. 2024 Oct 1 [cited 2025 Oct 7];4(4):372-94. Available from: https://www.mdpi.com/2673-8430/4/4/30. doi: 10.3390/biomed4040030.
- Tanzania Investment and Consultant Group Ltd. Why Tanzania Should Focus on Economic Independence Amid Declining Foreign Aid [Internet]. Dar es Salaam (Tanzania): Economic Research Centre; 2025 Mar 26 [cited 2025 Oct 6]. Available from: https://ticgl.com/why-tanzania-should-focus-on-economic-independence-amid-declining-foreign-aid/.
- Ministry of Health of Tanzania. National Guideline for Laboratory Sample Referral System: The use of a comprehensive sample referral system and laboratory hub-and-spoke model in TB, HIV, measles, and polio in Tanzania [Internet]. Dar es Salaam (Tanzania): Ministry of Health; 2019 Aug [cited 2025 Oct 6]. Available from: https://ntlp.go.tz/site/assets/files/1138/final_sample_referral_guideline.pdf.
- Centers for Disease Control and Prevention. HIV and TB Overview: Tanzania [Internet]. Atlanta (GA): CDC; 2025 Jul 15 [cited 2025 Oct 6]. Available from: https://www.cdc.gov/global-hiv-tb/php/where-we-work/tanzania.html.
