Review | Open Access | Volume 8 (3): Article 80 | Published: 30 Sep 2025
Strengthening emergency response in hard-to-reach settings through mobile Public Health Emergency Operation Centre
Menu, Tables and Figures
On Pubmed
On Google Scholar
Navigate this article
Tables
Table 1: Minimum list of items for mobile PHEOC
| Function | Equipment | Purpose/Use Case |
|---|---|---|
| Command & Coordination | Portable tents or inflatable shelters; container/vehicle-based units | Establish temporary or scalable field command posts |
| Foldable whiteboard + portable projector | Briefings, situational updates, and incident action planning | |
| Headsets, microphones, webcams | Virtual coordination and remote participation | |
| Data & Information Management | Rugged laptops and tablets with pre-installed emergency software and other solutions (Mobile electronic health records & surveillance platforms), wireless keyboard and mouse | Case management, line-listing, data entry, and dashboards, scanning and editing |
| Portable multifunction printer | Printing reports, scanning field documents, supporting documentation | |
| GIS-enabled tablets / mapping tools | Outbreak mapping, hotspot visualization, and logistics tracking | |
| Communication & Connectivity | Satellite phones, VHF/UHF radios | Reliable communication in no-network or disaster zones |
| Mobile Wi-Fi router / modem | Internet access in low-connectivity areas | |
| Encrypted messaging apps / portable servers | Secure information exchange and interoperability with national PHEOCs | |
| Portable video conferencing equipment | Remote meetings and coordination in the field | |
| Power & Infrastructure | Solar inverters (10,000w), hybrid inverters | Renewable and stable power supply for ICT systems |
| Batteries (12V, 200AH gel or lithium); small UPS | Continuous operations, backup for critical devices | |
| Portable solar panels / generators | Field-ready power sources for remote environments | |
| Logistics & Field Support | Compact vaccine/medical cooler | Safe storage of vaccines, samples, and temperature-sensitive supplies |
| Portable first-aid and responder welfare kits | Staff safety, health, and resilience in prolonged deployments | |
| Basic lighting and extension kits | Supporting 24/7 operations and flexible workspace setup |
Table 1: Minimum list of items for mobile PHEOC
Figures
Keywords
- Mobile Public Health Emergency Operations Centres (PHEOCs)
- Public Health Outbreak
- Response
- Hard-to-reach settings
- Emergency
- Preparedness
- Mobile PHEOC
&Corresponding author: Michael Sileshi Mekbib, Independent Researcher, Atlanta, Georgia, United States, Email: mikiethio@gmail.com ORCID: https://orcid.org/0009-0002-2888-690X
Received: 16 Jun 2024, Accepted: 29 Sep 2025, Published: 30 Sep 2025
Domain: Field Epidemiology, Public Health Emergency Response
Keywords: Mobile Public Health Emergency Operations Centres (PHEOCs), Public Health Outbreak, Response, Hard-to-reach settings, Emergency, Preparedness, Mobile PHEOC
©Michael Sileshi Mekbib et al. Journal of Interventional Epidemiology and Public Health (ISSN: 2664-2824). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Michael Sileshi Mekbib et al., Strengthening emergency response in hard-to-reach settings through mobile Public Health Emergency Operation Centre. Journal of Interventional Epidemiology and Public Health. 2025;8(3):80. https://doi.org/10.37432/jieph-d-25-00139
Abstract
Introduction: In many African countries, the effectiveness of outbreak response is hampered by the limited reach of Public Health Emergency Operations Centers (PHEOCs), which are often centralized and inaccessible to remote or underserved populations. This “last-mile coordination gap” contributes to delayed decision-making, inadequate resource mobilization, and increased morbidity during public health emergencies. To address this, we introduce the concept of a mobile PHEOC, a portable, field-deployable unit designed to replicate core PHEOC functions at the subnational and remote settings.
Methods: This conceptual paper is based on a structured literature review, comparative analysis of global and regional emergency coordination models, and synthesis of outbreak response experiences in Africa. Technical features and operational functions were adapted from the World Health Organization (WHO) PHEOC framework for resource-constrained environments.
Results: Evidence from 29 sources confirms that while 80% of African countries have established PHEOCs, only 29% are fully functional. National centers are often bureaucratic, infrastructure-intensive, and geographically distant from outbreak sites. Decentralized initiatives such as Nigeria’s subnational PHEOCs (which reduced outbreak response time from 10 to 3 days) and Africa CDC’s Incident Management Support Teams in the DRC (supporting deployment of 265,000 mpox vaccine doses), demonstrate the value of field-based coordination. Building on these models, the mobile PHEOC design integrates portable infrastructure (tents, solar-powered ICT), lean command structures based on Incident Management System (IMS), offline-capable digital tools, and codified governance frameworks to extend strategic coordination directly to outbreak sites. This model offers significant operational advantages by facilitating timely data-driven decisions, enhancing coordination between local and national levels, and strengthening community engagement during public health emergencies.
Conclusion: The mobile PHEOC is a portable, rapidly deployable system designed to improve emergency response in Africa’s rural and fragile settings by bridging coordination gaps between central command and frontline teams. It enhances timeliness, equity, and data-driven decision-making while engaging communities and local health actors. However, challenges such as sustained funding, equipment maintenance, security in fragile settings, and integration with national health systems must be addressed. To maximize its effectiveness, mobile PHEOCs should be institutionalised within national frameworks, supported by a costed funding plan, interoperable digital systems, and rosters of trained personnel. Evaluation and pilot studies are needed to refine and scale the model for diverse public health threats.
Introduction
The frequency, complexity, and impact of public health emergencies have increased markedly in recent decades, driven by factors such as globalization, climate change, population growth, and increased mobility [1-3]. From pandemics like COVID-19 to regional outbreaks such as Ebola in West Africa, Mpox in Democratic Republic of Congo (DRC) and cholera in Haiti, the world continues to face health threats that demand fast, coordinated, and context-sensitive responses [1,4]. Central to this capacity is the Public Health Emergency Operations Center (PHEOC) , a standardized hub for multisectoral coordination, situational awareness, and emergency decision-making [4,5].
Despite the establishment of national PHEOCs in many countries, subnational and remote regions often lack comparable capacities, resulting in delayed responses, inefficient resource deployment, and increased morbidity and mortality [5-7]. In numerous African countries, while national PHEOCs existed, they struggled to support real-time operations in rural districts, where poor internet connectivity, inadequate infrastructure, and fragmented data systems hindered effective coordination [4,5]. The COVID-19 pandemic exposed the structural weaknesses in emergency response systems across both high- and low-income countries [8]. Similarly, during the 2014–2016 Ebola outbreak, centralised PHEOCs helped shape national strategies, but ground-level coordination in outbreak epicentres was often ad hoc or entirely absent, exacerbating crises in remote communities [9].
There is growing recognition that decentralized and flexible models of emergency response are essential, especially in low-resource settings [6,10,11]. The Joint Emergency Preparedness and Response Action Plan (JEAP), a strategic collaboration between World Health Organization (WHO) and the Africa Centres for Disease Control and Prevention (Africa CDC), prioritises strengthening sub-regional coordination and logistics to enhance Africa’s rapid health emergency response. The plan establishes regional hubs to preposition essential medical supplies, ensuring faster deployment and reducing delivery times to 24–48 hours. [12]. To this end, innovations such as mobile command posts, field operations tents, and mobile data hubs have emerged in humanitarian and emergency health sectors, but these have largely focused on logistics and clinical care, not the strategic command-and-control functions typically associated with a PHEOC [10,12].
A fully functional PHEOC serves as the central hub for managing health emergencies by facilitating structured coordination, decision-making, and communication. According to the WHO, the core functions of a PHEOC include coordinating incident management (including command structure and task assignments); collecting, analyzing, and sharing surveillance and field data; managing logistics and resources, such as vaccine stockpiles, emergency supplies, and responder deployments; ensuring timely risk communication and public information dissemination; and integrating with national and international response systems for unified action. These functions are supported by trained personnel, interoperable information systems, and robust infrastructure. When adapted to mobile or decentralised formats, such as the mobile PHEOC, these same core functions can be replicated in the field to maintain operational continuity during emergencies [12].
Despite global advances in public health preparedness, many low- and middle-income countries (LMICs) face significant challenges in effectively coordinating and implementing emergency response at the subnational level [7,11]. While national PHEOCs have been established in numerous countries as part of the International Health Regulations (IHR 2005) core capacities, their functionality is often centralized, with limited reach to rural, remote, or underserved populations [6,7,13]. The West African Ebola outbreak (2014–2016) revealed critical weaknesses at the district level, which significantly hindered effective response [14]. Weak district-level coordination contributed to delays in contact tracing, misallocation of resources, and poor community engagement, all of which contributed to the rapid spread of the virus in rural areas [15]. Structural challenges of centralized coordination included fragmented communication lines, overlapping command structures, and limited decision-making authority at subnational levels [16]. Similarly, during the COVID-19 pandemic, district and county health officials across several African countries lacked the tools, authority, and infrastructure to operate autonomously, resulting in dependency on national command structures and slower responses to emerging threats [6, 8].
Traditional PHEOCs are fixed-location command centers, often based in capital cities or major urban areas. While they provide valuable strategic oversight, they are not designed for immediate deployment or use in areas with poor infrastructure, particularly during outbreaks or emergencies affecting remote districts, mobile populations, or refugee settings [4, 5, 17]. As a result, many countries face what has been described as a “last-mile coordination gap”, the inability to bring command-and-control capacity directly to the outbreak sites [3, 6, 18].
Public health emergencies are becoming more complex and frequent. From vector-borne outbreaks like dengue and chikungunya to zoonotic threats such as Marburg virus and Rift Valley fever, emergencies now often arise in rural or borderland zones with limited surveillance and coordination infrastructure [5,9]. Climate change, displacement, and urbanization further complicate response efforts, increasing the need for agile, field-based coordination models that can operate beyond static, city-based systems [4,6].
This paper introduces the concept of a mobile PHEOC, a compact, field-deployable unit designed to deliver the critical functions of a PHEOC in decentralized settings. Unlike static, facility-based PHEOCs, this mobile unit can be rapidly deployed to outbreak hotspots, refugee camps, disaster zones, or underserved rural districts, enabling local authorities to coordinate responses with real-time data, digital tools, and communication systems.
We aim to outline the justification, design, operational approach, and potential impact of the mobile PHEOC model. Drawing on lessons from past public health emergencies and emerging best practices in digital health innovation, we argue that mobile PHEOCs are both feasible and essential for strengthening emergency response systems, particularly in the global south.
Methods
Study Design
This study employed a conceptual and narrative synthesis approach drawing on secondary data from peer-reviewed publications and technical reports. The methodology was designed to: (i) assess limitations of centralized PHEOCs, (ii) identify practical decentralized and mobile emergency management initiatives, and (iii) propose a design for a mobile PHEOC that integrates lessons from static PHEOCs and global experiences.
Literature search and Evidence Synthesis
A comprehensive search was conducted between June and September 2025 across multiple electronic databases, including PubMed and Web of Science, complemented by technical reports from WHO, Africa CDC, and the U.S. CDC. The combined Boolean search string was:
(“Public Health Emergency Operations Center” OR PHEOC OR “Incident Management System” OR IMS) AND (“Mobile emergency operations center” OR “Mobile command center” OR “Portable command post” OR “Field-deployable PHEOC”) AND (“Decentralized emergency response” OR “Subnational emergency coordination” OR “District-level emergency management”) AND (“Field-based coordination” OR “On-site emergency management” OR “Frontline outbreak response”).
Articles were screened based on the following criteria:
- Inclusion: Publications and technical reports from 2015-2025 that described the design, deployment, or operationalization of mobile or subnational PHEOCs; studies from all geographic regions; English-language publications; evidence relevant to public health emergencies, outbreaks, or pandemics.
- Exclusion: Studies that focused on non-health-related emergency operations, or publications lacking sufficient methodological detail.
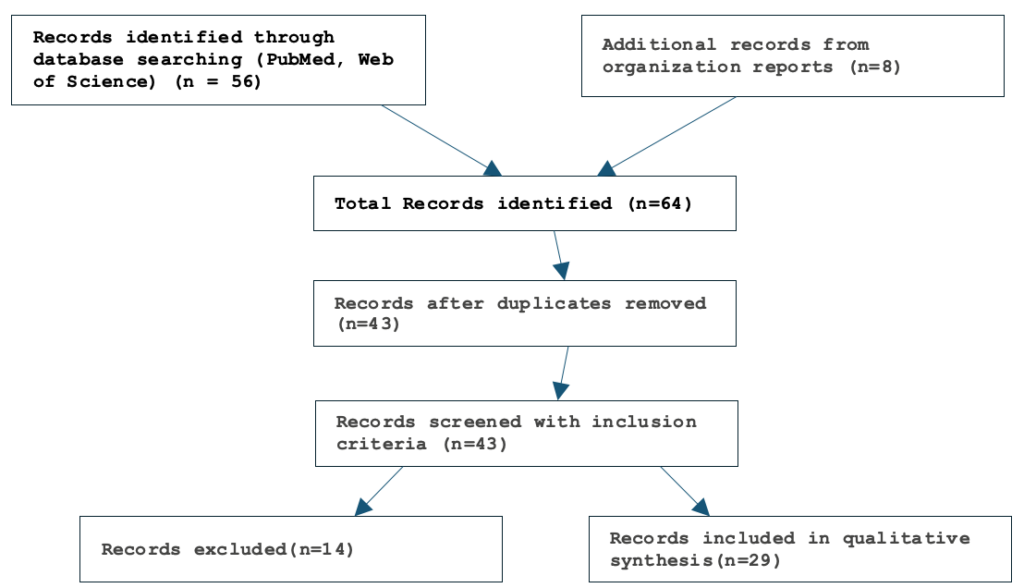
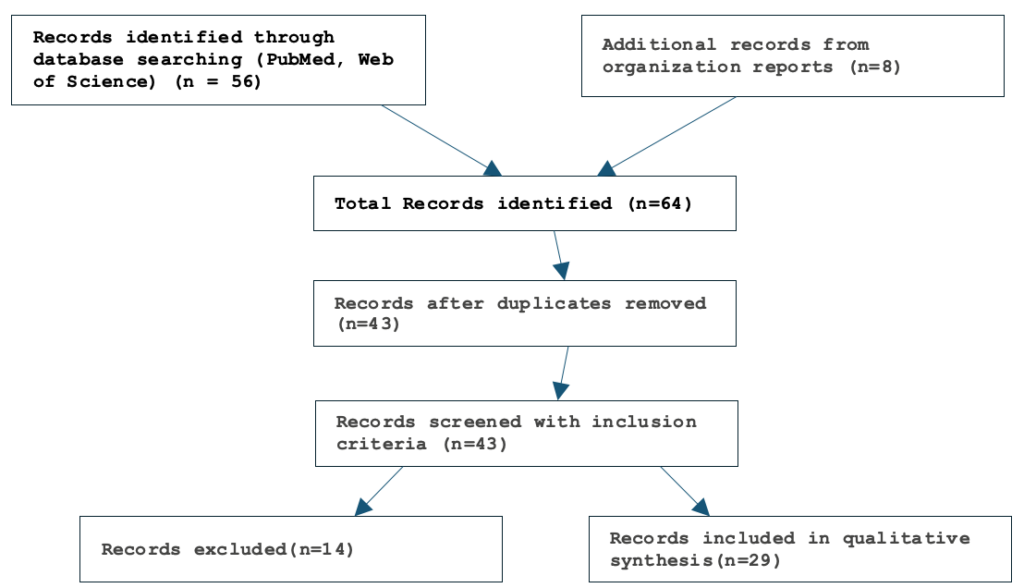
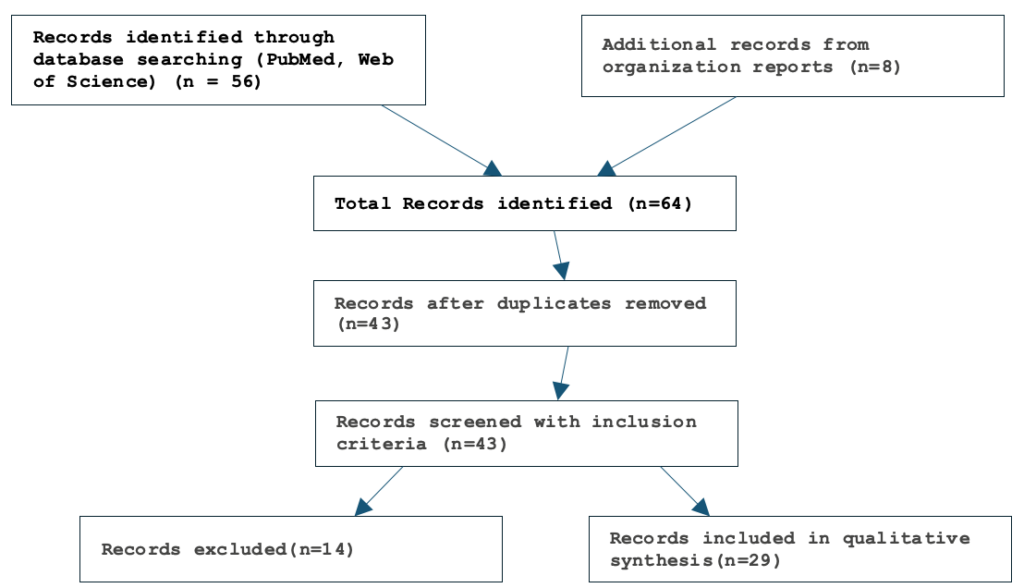
After removal of duplicates, titles and abstracts of identified records were screened independently by two reviewers based on the above criteria. Full texts of potentially relevant documents were further assessed for eligibility. Discrepancies were resolved through discussion. This process resulted in a final corpus of 29 articles and reports included for synthesis (Figure 1).
To contextualize findings, a comparative case review was conducted on mobile and decentralized emergency response models. Examples included mobile EOCs in disaster response, humanitarian field coordination tents, and portable digital hubs in health emergencies. Each case was analyzed for deployment context, operational functions, technologies, strengths, and limitations, and the insights were used to refine the mobile PHEOC model.
Drawing on the literature synthesis and case review, a mobile PHEOC design was proposed to adapt the core functions of static PHEOCs’ command and coordination, surveillance and data management, logistics, communication, and stakeholder engagement into a field-deployable format.
Results
Static PHEOCs and their Limitations
PHEOCs are critical hubs for coordinating outbreak responses, but traditional static, centralized PHEOCs often struggle in low-resource or geographically dispersed settings. The majority of such PHEOCs are national-level and resource-intensive, making them slow or underused at subnational levels [5,19,20]. For example, a cross-sectional study in Africa found that while 80% of countries had PHEOCs, only 29% were fully functional, with many lacking legal authority and connectivity [19].
Moreover, centralized systems can become bureaucratic and inflexible, delaying decisions when local outbreaks demand rapid action [5,21]. These limitations have driven interest in decentralized and mobile models that bring emergency management closer to outbreak sites. In this review, we synthesize findings from 29 sources on the limitations of centralized PHEOCs [1], practical decentralized/mobile initiatives [2], and design considerations for a mobile PHEOC, to guide policymakers considering mobile PHEOC adoption [3].
Centralized PHEOCs, while essential for national coordination, exhibit several well-documented limitations that can hinder rapid and effective outbreak response. One key challenge is their bureaucratic structure and slow decision-making. Many PHEOCs operate under rigid Incident Management Systems (IMS) with hierarchical decision chains, which can delay adaptive responses in fast-moving emergencies [5,21]. For example, respondents in Sierra Leone’s Ebola response reported that national EOCs suffered from cumbersome processes and weak links to districts, slowing funding disbursement and field-level action [21].
High resource and infrastructure demands pose another constraint. Static PHEOCs require substantial investments in physical facilities, information and communications technology, power, and staffing. In low-resource settings, such requirements are often described as “an unaffordable luxury” [20,22]. Many African PHEOCs have reported inadequate funding, unreliable electricity, and insufficient equipment [19,20]. Early COVID-era situation rooms in Nigeria and Turkey exemplified these limitations, beginning as small, poorly equipped spaces lacking adequate audiovisual capabilities [20].
Coordination and communication breakdowns are also common. Central hubs can create overlapping responsibilities, unclear roles, and poor information flow, leading to duplicated efforts and confusion among field teams [21,23]. Even when focal points are designated, urgent case data often must pass through central approvals, slowing cross-border updates (27). Interoperability remains a chronic issue, as many national PHEOCs rely on heterogeneous IT systems, while rural areas frequently lack reliable internet connectivity [21,22,24].
Geographic inflexibility further limits effectiveness. Static centers are often distant from outbreak sites, delaying critical actions such as sample transport or intervention deployment. In Uganda’s Ebola response, long-distance sample shipments delayed confirmation [14,15], and in the DRC, insecurity and challenging terrain slowed shipments to central laboratories [14].
Governance and legal gaps compound these challenges. Many countries lack formal mandates that empower PHEOCs to coordinate multisectoral responses. Studies indicate that only 40–60% of African countries have enacted legal frameworks or multihazard plans [19,20,22]. Without clear authority and governance structures, PHEOCs struggle to mobilise resources and coordinate effectively across sectors [12,16].
Human resource and training shortfalls are pervasive. Many PHEOCs operate with small core teams and few dedicated responders, with surveys revealing inadequate training and a lack of routine simulations in most centers [19,20]. Frequent staff turnover, such as observed in Nigeria, further disrupts operations [20].
Finally, limited flexibility and reach restrict PHEOCs’ ability to address localized needs. Fixed vaccination sites, for example, often fail to reach hesitant or low-mobility populations, whereas mobile vaccination units have proven successful [15]. Natural disasters, such as the floods in Malawi, have also demonstrated that centralized dispatch can increase response times when infrastructure is compromised [12].
Decentralized and Mobile Public Health Emergency Management Experiences
The concept of mobile or decentralized emergency response is not entirely new. Various models have been implemented across the globe, particularly by military, humanitarian, and disaster response agencies. However, most of these models focus on clinical response (e.g., mobile clinics, field hospitals) or logistical operations, and few fully replicate the strategic coordination and command functions of a PHEOC.
Global and Regional Experiences
International public health agencies have demonstrated the value of combining centralized PHEOCs with mobile field teams to enhance outbreak response. The WHO has long supported mobile field teams that deploy to outbreak sites for surveillance and case investigation. While these teams provide essential response services, they often report back to centralized PHEOCs rather than conducting full operational coordination onsite [19]. WHO’s PHEOC Framework calls for a central coordination hub while maintaining field-deployable Emergency Mobile Medical Teams (eMMTs) at national and subnational levels. In South Sudan, these self-sufficient mobile teams conducted outbreak investigations, rapid assessments, and emergency interventions, reporting through the central PHEOC structure to augment broader health-cluster responses [12]. This approach illustrates how centralized coordination can support rapid, flexible field operations.
Africa CDC has implemented one of the continent’s clearest examples of mobile emergency coordination through the deployment of its Incident Management Support Team (IMST) to the Democratic Republic of the Congo (DRC) in response to the 2024–2025 mpox outbreak. Unlike traditional support missions, this IMST served as an on-the-ground public health command structure, working directly with the DRC’s Ministry of Health to enhance coordination, surveillance, and operational oversight [31]. This deployment represents a unique adaptation of the PHEOC model, bringing not only technical support but also strategic decision-making, coordination, and vaccine deployment capabilities directly to the field. The IMST facilitated the rollout of more than 265,000 doses of the mpox vaccine in 12 high-priority health zones, and supported contact tracing, laboratory diagnostics, and real-time situation reporting [32,33].
Tangible results include increased vaccine uptake among frontline workers and high-risk populations, improved multi-level coordination through an in-country Technical Review Committee, and more structured epidemiological reporting systems [31]. Despite challenges such as ongoing conflict in eastern provinces, the field-based coordination model enabled more responsive action and positioned Africa CDC as a continental leader in scalable emergency operations [31,32]. Africa CDC’s IMST functions as a portable, human-resource-driven, mobile PHEOC, designed for adaptability in low-resource, high-complexity settings, closely aligning with the concept of the mobile PHEOC.
Médecins Sans Frontières (MSF) complements these government-led efforts with specialized rapid-deployment units designed for immediate field operations during high-impact emergencies. Mobile units, including Cholera Treatment Centres (CTCs), Ebola Treatment Units (ETUs), and Mobile Unit Surgical Trailers (MUST), can be established within hours and integrated with local and national PHEOCs. For instance, during cholera outbreaks, CTCs deliver essential care and conduct mass vaccination campaigns, while MUST units provide operating theatres, and supply storage for trauma and surgical care. In Ebola outbreaks, ETUs operate in coordination with WHO and national PHEOCs, ensuring structured field-based patient care alongside real-time reporting to central command [34-36]. Collectively, these examples demonstrate how deployable field assets extend the operational reach of PHEOCs, allowing timely emergency management directly at outbreak sites.
Countries Experiences
In many African countries, timely outbreak response has often been hindered by logistical, geographic, and infrastructural constraints. The deployment of mobile response teams and decentralized coordination mechanisms functionally equivalent to mobile PHEOCs has emerged as a crucial strategy for improving outbreak management in hard-to-reach or resource-limited settings. Several African countries have demonstrated the value of subnational PHEOCs and mobile response mechanisms in improving outbreak management.
In Nigeria, state-level PHEOCs reduced average outbreak response time from 10 days to 3 days [20], while Sierra Leone’s District Ebola Response Centers enhanced operational reach across districts [21]. Similarly, Ethiopia and Kenya established regional task forces and county disaster committees, strengthening vertical data flow and improving coordination for rapid mobilization of resources [23].
Mobile and field-based response units have complemented these subnational structures. WHO-supported Emergency Mobile Medical Teams (eMMTs) in South Sudan are capable of deploying within 24–48 hours to fill health service gaps [13]. In conflict and disaster settings, mobile clinics and trauma stabilization points have provided rotating, site-based services, ensuring continuity of care even in unstable environments [12]. Mobile laboratories and container-based medical stations have further accelerated response times; for instance, Uganda and DRC deployed mobile labs during Ebola outbreaks to reduce diagnostic turnaround, while Taiwan utilized container-based epidemic stations to manage COVID-19 surges [14,15].
Advances in technology and communication tools have also enhanced subnational PHEOC operations. Mobile health (mHealth) applications facilitate surveillance, triage, logistics, and health education [11], while informal communication platforms such as WhatsApp and Facebook have enabled faster coordination during emergencies [8]. The use of unmanned aerial vehicles (UAVs) for medical delivery and surveillance has also been piloted, further extending the reach of field operations [11].
Virtual networks and capacity-building initiatives have supported peer mentorship and real-time experience sharing across PHEOCs. During the COVID-19 pandemic, online platforms and multilingual webinars allowed knowledge transfer and training across jurisdictions [10], while ASEAN countries held annual cross-border tabletop exercises to strengthen regional preparedness [8].
Finally, community and intersectoral engagement have been crucial for effective outbreak response. Local leaders, community health workers, and civil society actors have contributed to surveillance and response activities in countries such as Kenya, Ethiopia, and India [9]. Mobile units often co-locate services with existing clinics to reduce stigma and improve community access to care [12].
Proposed Design and Operational Considerations for Mobile PHEOCs
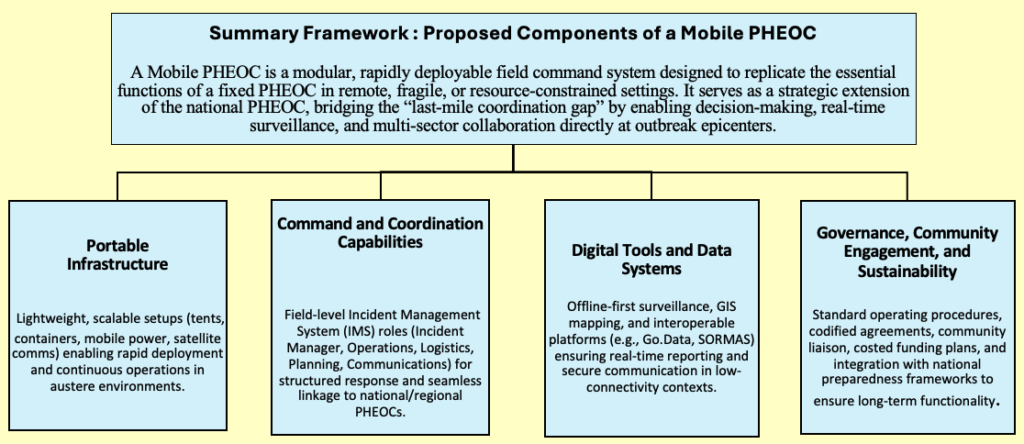
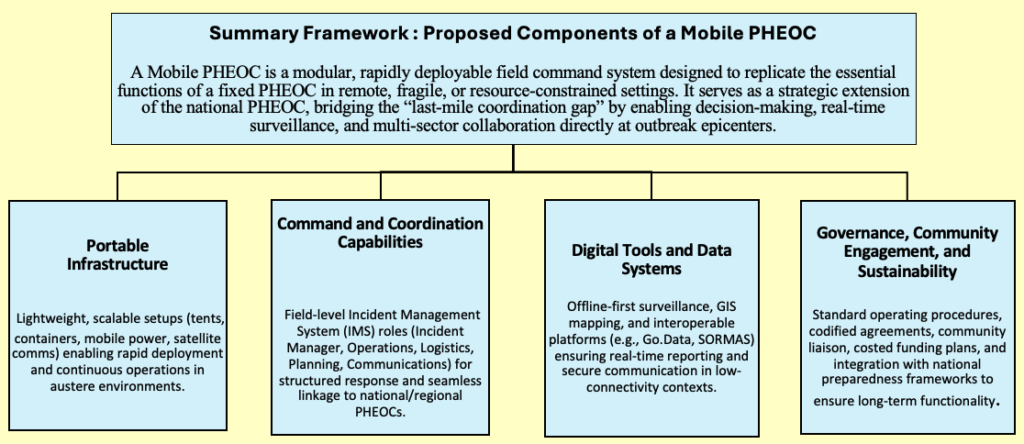
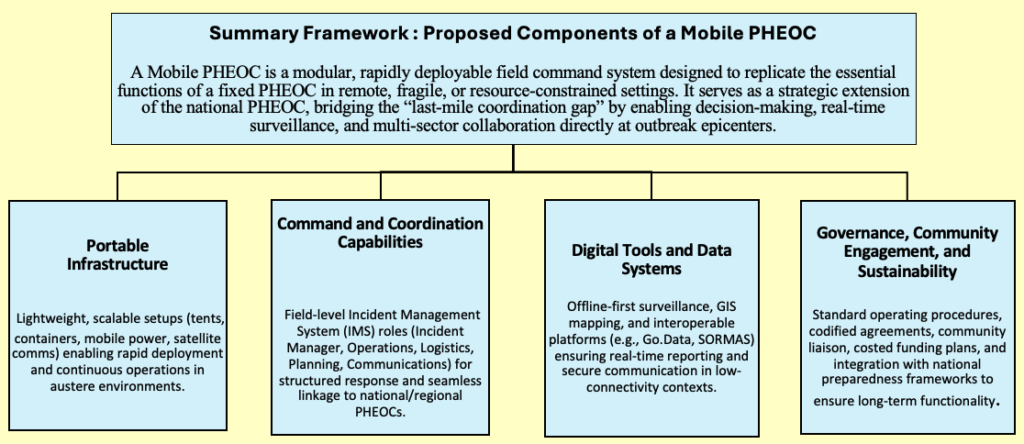
A mobile PHEOC can be conceptualized as a modular, field-deployable command system that mirrors the essential functions of a national PHEOC while adapting them for rapid deployment in remote, resource-limited, or fragile settings. The mobile PHEOC integrates four interconnected pillars: (i) portable infrastructure that allows rapid physical setup and reliable power/connectivity; (ii) command and coordination capabilities modeled on the Incident Management System (IMS), ensuring structured leadership and decision-making in the field; (iii) digital tools and data systems designed for real-time surveillance, outbreak mapping, and secure communication even in low-connectivity environments; and (iv) governance, community engagement, and sustainability mechanisms that align operations with national frameworks, standard operating procedures, and local ownership (Figure 2).
Together, these elements allow the mobile PHEOC to function not just as a temporary support unit, but as a strategic extension of the national PHEOC, bridging the “last-mile coordination gap” by bringing decision-making authority, situational awareness, and resource management closer to outbreak epicenters.
Portable Infrastructure: The foundation of the proposed mobile PHEOC is a lightweight, field-ready and modular-based infrastructure designed for low-resource and hard-to-reach environments, which can be expanded based on local context (Table 1). It can be transported by car, motorbike, or even on foot, enabling rapid deployment within 2-6 hours by a small team of 4-6 personnel with basic emergency management training [12]. For larger, prolonged, or multi-hazard emergencies, container- or vehicle-based units are recommended to transport heavier equipment and provide a secure workspace.
The infrastructure includes rugged laptops and tablets with pre-installed health emergency software and offline functionality, satellite communication tools for internet access in areas without mobile networks, and mobile power sources such as solar panels and high-capacity battery packs. To support physical setup, foldable tents or inflatable shelters are included for establishing temporary command posts. VHF/UHF radios enable interagency communication where cellular connectivity is unavailable [12,14].
Command and Coordination Capabilities: The Mobile PHEOC replicates the Incident Management System (IMS) structure endorsed by WHO and Africa CDC, enabling clear role assignments [23,37]. Its lean command structure allows rapid activation of response pillars, surveillance, logistics, risk communication and supports field-level authority while maintaining strong liaison mechanisms with national PHEOCs. Integrated dashboards and decision-support tools provide real-time metrics for effective outbreak control even in disconnected or resource-limited settings [6,7,11,12]. Deployment teams should be drawn from a pre-identified national or subnational roster of trained personnel, ensuring readiness and minimizing ad hoc staffing gaps. It manages surveillance, case investigation, logistics, and risk communication on the ground while maintaining real-time links with national and regional PHEOCs for strategic decision-making.
Digital Tools and Data Systems: Robust data collection and analysis are central to mobile PHEOC operations. Systems are compatible with case-based surveillance, line listing, mobile data collection platforms (e.g., KoboToolbox, ODK), and GIS-enabled offline data capturing and mapping for outbreak visualisation and logistics tracking. Where feasible, integration with national and regional platforms such as eIDSR, Go.Data and SORMAS ensure timely reporting to central PHEOCs. Offline-first apps and redundant communication channels, including encrypted messaging and satellite links, maintain operational continuity in areas with limited connectivity [6,7,11,12].
The digital tools need to be designed with a strong focus on usability by local responders, ensuring it can be effectively operated in diverse field settings. It features multilingual interface options to accommodate local language needs, step-by-step deployment manuals, and quick-start guides for ease of setup. Additionally, embedded training videos support just-in-time learning [12,19,23], enabling rapid orientation and operation by field teams with varying levels of technical expertise. This design ensures that local health departments or local NGOs can own and operate the PHEOC with minimal external support.
To safeguard data privacy within mobile PHEOCs, operations follow the core principles of national PHEOCs, emphasizing centralized data storage, password-protected offline mobile tools, and user authentication to reduce risks of breaches in insecure settings. Mobile units function primarily as data collectors, syncing securely with central PHEOCs where official data storage and management occur, thus minimizing exposure in the field. This aligns with WHO’s PHEOC framework that stresses standardized protocols for confidentiality and secure information flow [19], while practical experiences highlight the importance of strengthening digital tools, offline-first applications, and clear reporting mechanisms for reliability in unstable areas [11, 12, 20].
Governance, Community Engagement, and Sustainability: Effective mobile PHEOCs operate within codified governance frameworks and Memorandum of Understanding (MOUs) for cross-sectoral collaboration, with standardised Standard Operating Procedures (SOPs) for data sharing [6,12,19]. Field engagement emphasises risk communication, liaison with local leaders and community health workers [6, 12, 23]. Designs consider generic applicability, integration with national plans, dual-use functionality, and cost-effectiveness assessments to ensure long-term sustainability [12,13,20].
In sum, mobile PHEOCs extend the reach of emergency management to outbreak epicenters and underserved areas, combining portable infrastructure, interoperable systems, structured command, and field-adapted tools to deliver timely, coordinated, and context-sensitive public health responses.
Discussion
This review highlights the growing need for flexible, field-deployable PHEOCs to complement traditional, centralized systems. Centralized PHEOCs, while critical for national oversight and strategic coordination, have well-documented limitations in timeliness, reach, and adaptability. Bureaucratic decision-making, high resource demands, geographic inflexibility, and gaps in governance and staffing constrain the ability of static PHEOCs to respond effectively to outbreaks in remote or underserved regions [5,21]. Evidence from Sierra Leone’s Ebola response demonstrates that hierarchical structures and centralized authority can delay critical interventions, highlighting the “last-mile coordination gap” that hampers rapid outbreak control [21].
By contrast, mobile and decentralized PHEOC models offer a feasible and practical solution to these challenges. Mobile PHEOCs, as demonstrated in WHO-supported Emergency Mobile Medical Teams (eMMTs) in South Sudan, Africa CDC’s IMST deployments in DRC, and MSF rapid-deployment units, provide agile, field-based coordination that brings decision-making and operational capacity directly to the outbreak site. Evidence from Nigeria (reduced outbreak response time from 10 to 3 days) and Africa CDC’s IMST deployment in DRC (coordinating 265,000 mpox vaccine doses) demonstrates the feasibility and added value of decentralised coordination [12,13,30,32]. These units are designed to replicate core PHEOC functions, including incident management, data collection, logistics, and risk communication while operating with minimal infrastructure and personnel. The portable design, integration of offline-first digital tools, and structured but lean command systems make mobile PHEOCs feasible even in resource-constrained or conflict-affected settings [6,7,11,12].
Comparing country experiences further underscores their importance. Subnational EOCs in Nigeria, Sierra Leone, Ethiopia, and Kenya reduced response times, improved vertical data flow, and strengthened operational reach [20,21,23]. Mobile units such as field laboratories and container-based epidemic stations in Uganda, DRC, and Taiwan further illustrate the feasibility of extending PHEOC capabilities to peripheral regions while maintaining data integrity and connectivity with national command centers [14,15]. Technology-enabled solutions, including mHealth platforms, GIS mapping, and UAV-supported logistics, further enhance the operational efficiency of mobile PHEOCs and facilitate real-time reporting [8,11].
The mobile PHEOC approach addresses the limitations of centralized systems by providing speed, flexibility, and field-level autonomy. Unlike static centers, mobile units can be rapidly deployed within hours, are operable by small multidisciplinary teams, and integrate community engagement and context-sensitive strategies [12,14]. This not only accelerates outbreak detection and response but also improves equity by reaching populations often neglected by traditional systems. Moreover, mobile PHEOCs provide a platform for testing innovative digital tools, cross-border collaboration, and multi-hazard preparedness, contributing to broader resilience in health systems [12,13,20].
Feasibility is further supported by evidence from global practice: WHO’s guidelines emphasise centralised coordination with mobile field teams, while CDC and Africa CDC experience demonstrates operational scalability and interoperability in diverse contexts [12,30]. MSF rapid deployment units exemplify the integration of clinical, logistical, and command functions in mobile field units, illustrating the capacity of mobile PHEOCs to provide structured coordination alongside service delivery [31,32].
Despite their promise, mobile PHEOCs face several operational challenges that can affect successful implementation. Effective deployment requires robust legal and governance frameworks that clearly define authority, responsibilities, and mechanisms for cross-sector collaboration [6,12,19]. Operational feasibility is also constrained by logistics, security, and human resource limitations, particularly in conflict-affected, remote, or low-resource settings where baseline infrastructure, trained personnel, and reliable supply chains may be lacking [12,23]. Integration with national health systems, interoperability with centralized PHEOCs, and standardization of digital tools are critical to ensure mobile operations complement rather than duplicate existing emergency response structures [6,7,11,12]. Furthermore, technology-dependent components—including satellite communications, mobile data systems, and power sources—are susceptible to failures or connectivity issues, which can reduce operational effectiveness [12,14]. Sustainable funding, continuous workforce training, structured simulation exercises, and context-specific planning are therefore essential to maintain readiness, resilience, and the overall impact of mobile PHEOCs [12,23].
Importantly, mobile PHEOCs should not be viewed as replacements for central command but as complementary units. The balance between central oversight and field autonomy must be carefully managed, with interoperable systems and clear lines of authority.
Limitations
This study is primarily based on a synthesis of case reports, organizational documents, and published literature, which may limit the generalizability of findings across all contexts in Africa and other low-resource settings. Quantitative data on the direct impact of mobile PHEOCs on outbreak response times, morbidity, and cost-effectiveness are limited, and much of the evidence reflects short-term deployments or pilot initiatives. Additionally, variations in governance, infrastructure, digital interoperability, and human resource capacity across countries may influence the feasibility and operational success of mobile PHEOCs, which this study could not fully capture. Despite these limitations, the analysis provides a strategic overview of design considerations, operational advantages, and practical insights for implementing mobile PHEOCs in decentralized emergency response.
Conclusion
Mobile PHEOCs are a feasible and essential extension of public health emergency management, particularly in low-resource and geographically dispersed settings. By bridging the gap between centralized command centers and field operations, they enhance timeliness, flexibility, and equity in outbreak response. Evidence from multiple countries and organizations demonstrates that mobile PHEOCs improve real-time coordination, data-driven decision-making, and effective resource allocation, enabling district-level teams to operate independently even in low-connectivity, high-complexity environments. Their portable, field-adaptable design, combined with integrated digital tools and satellite communication, extends the core functions of traditional PHEOCs directly to the frontline, improving outbreak control and strengthening health security.
To ensure sustainable impact, mobile PHEOCs should be institutionalized within national emergency preparedness frameworks and supported through targeted investments in logistics, infrastructure, and workforce capacity. Simulation-based training, standardized deployment protocols, and multi-sector partnerships are critical to addressing operational and technical challenges. There is a need to develop a dedicated framework and operational handbook for mobile PHEOCs, building on the principles of the WHO Framework for a PHEOC, to provide context-specific guidance and best practices. Future research should evaluate their performance across varied contexts, including cross-border epidemics, to refine the model, enhance efficiency, and maximize health outcomes. Mobile PHEOCs thus offer a scalable, adaptable solution to strengthen decentralized emergency response and build resilient health systems.
What is already known about the topic
- Centralized PHEOCs play a vital role in outbreak coordination, but their limited reach to remote or underserved areas creates a “last-mile coordination gap.”
- While mobile response units exist, they often lack the strategic and operational capabilities of a full PHEOC, leading to delayed responses and fragmented field coordination during emergencies.
What this study adds
- This study presents the mobile PHEOC, a portable, rapidly deployable unit that replicates essential emergency coordination functions in low-resource settings.
- By integrating digital tools, mobile infrastructure, and field-adapted systems, it strengthens localized response, enhances data-driven decision-making, and bridges critical gaps between national command centers and frontline teams.
Authors´ contributions
Michael Sileshi Mekbib and Dennis Kibiye jointly conceptualized the study. Michael Sileshi Mekbib was responsible for data curation, formal analysis, methodology development, validation, and manuscript writing. Dennis Kibiye contributed to discussions and critically reviewed the manuscript. All authors have read and approved the final version of the manuscript.
| Function | Equipment | Purpose/Use Case |
|---|---|---|
| Command & Coordination | Portable tents or inflatable shelters; container/vehicle-based units | Establish temporary or scalable field command posts |
| Foldable whiteboard + portable projector | Briefings, situational updates, and incident action planning | |
| Headsets, microphones, webcams | Virtual coordination and remote participation | |
| Data & Information Management | Rugged laptops and tablets with pre-installed emergency software and other solutions (Mobile electronic health records & surveillance platforms), wireless keyboard and mouse | Case management, line-listing, data entry, and dashboards, scanning and editing |
| Portable multifunction printer | Printing reports, scanning field documents, supporting documentation | |
| GIS-enabled tablets / mapping tools | Outbreak mapping, hotspot visualization, and logistics tracking | |
| Communication & Connectivity | Satellite phones, VHF/UHF radios | Reliable communication in no-network or disaster zones |
| Mobile Wi-Fi router / modem | Internet access in low-connectivity areas | |
| Encrypted messaging apps / portable servers | Secure information exchange and interoperability with national PHEOCs | |
| Portable video conferencing equipment | Remote meetings and coordination in the field | |
| Power & Infrastructure | Solar inverters (10,000w), hybrid inverters | Renewable and stable power supply for ICT systems |
| Batteries (12V, 200AH gel or lithium); small UPS | Continuous operations, backup for critical devices | |
| Portable solar panels / generators | Field-ready power sources for remote environments | |
| Logistics & Field Support | Compact vaccine/medical cooler | Safe storage of vaccines, samples, and temperature-sensitive supplies |
| Portable first-aid and responder welfare kits | Staff safety, health, and resilience in prolonged deployments | |
| Basic lighting and extension kits | Supporting 24/7 operations and flexible workspace setup |
References
- Yang L, Fang X, Zhu J. Knowledge mapping analysis of public health emergency management research based on web of science. Front Public Health [Internet]. 2022 Mar 9 [cited 2025 Sep 30];10:755201. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.755201/full doi: 10.3389/fpubh.2022.755201
- Wen C, Liu W, He Z, Liu C. Research on emergency management of global public health emergencies driven by digital technology: a bibliometric analysis. Front Public Health [Internet]. 2023 Jan 11 [cited 2025 Sep 30];10:1100401. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1100401/full doi: 10.3389/fpubh.2022.1100401
- Morens DM, Fauci AS. Emerging pandemic diseases: how we got to COVID-19. Cell [Internet]. 2020 Sep 3 [cited 2025 Sep 30];182(5):1077-92. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0092867420310126 doi: 10.1016/j.cell.2020.08.021
- Ma J, Huang Y, Zheng ZJ. Leveraging the public health emergency operation center (PHEOC) for pandemic response: opportunities and challenges. Glob Health J [Internet]. 2020 Dec 4 [cited 2025 Sep 30];4(4):118-20. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2414644720300579 doi: 10.1016/j.glohj.2020.11.004
- Allen T, Spencer R. Barriers and enablers to using an emergency operations center in public health emergency management: a scoping review. Disaster Med Public Health Prep [Internet]. 2023 Jun 9 [cited 2025 Sep 30];17:e407. Available from: https://www.cambridge.org/core/product/identifier/S1935789323000502/type/journal_article doi: 10.1017/dmp.2023.50
- Oyebanji O, Ibrahim Abba F, Akande OW, Aniaku EC, Abubakar A, Oladejo J, et al. Building local capacity for emergency coordination: establishment of subnational Public Health Emergency Operations Centres in Nigeria. BMJ Glob Health [Internet]. 2021 Oct 28 [cited 2025 Sep 30];6(10):e007203. Available from: https://gh.bmj.com/lookup/doi/10.1136/bmjgh-2021-007203 doi: 10.1136/bmjgh-2021-007203
- Elmahal OM, Abdullah A, Elzalabany MK, Anan HH, Samhouri D, Brennan RJ. Public health emergency operation centres: status, gaps and areas for improvement in the Eastern Mediterranean Region. BMJ Glob Health [Internet]. 2022 Jun 28 [cited 2025 Sep 30];7 Suppl 4:e008573. Available from: https://gh.bmj.com/lookup/doi/10.1136/bmjgh-2022-008573 doi: 10.1136/bmjgh-2022-008573
- Tessema GA, Kinfu Y, Dachew BA, Tesema AG, Assefa Y, Alene KA, et al. The COVID-19 pandemic and healthcare systems in Africa: a scoping review of preparedness, impact and response. BMJ Glob Health [Internet]. 2021 Dec 1 [cited 2025 Sep 30];6(12):e007179. Available from: https://gh.bmj.com/lookup/doi/10.1136/bmjgh-2021-007179 doi: 10.1136/bmjgh-2021-007179
- Boland ST, Polich E, Connolly A, Hoar A, Sesay T, Tran AMA. Overcoming operational challenges to Ebola case investigation in Sierra Leone. Glob Health Sci Pract [Internet]. 2017 Jul 27 [cited 2025 Sep 30];5(3):456-67. Available from: http://www.ghspjournal.org/lookup/doi/10.9745/GHSP-D-17-00126 doi: 10.9745/GHSP-D-17-00126
- Roland Akoh N. The effectiveness of decentralisation as a response mechanism for disaster risk management in Bamenda, North West Cameroon. LARP [Internet]. 2018 May 25 [cited 2025 Sep 30];3(2):51. Available from: http://www.sciencepublishinggroup.com/journal/paperinfo?journalid=241&doi=10.11648/j.larp.20180302.15 doi: 10.11648/j.larp.20180302.15
- Wang Y, Li J, Zhao X, Feng G, Luo X. Using mobile phone data for emergency management: a systematic literature review. Inf Syst Front [Internet]. 2020 Jun 16 [cited 2025 Sep 30];22(6):1539-59. Available from: https://link.springer.com/10.1007/s10796-020-10057-w doi: 10.1007/s10796-020-10057-w
- McGowan CR, Baxter L, Deola C, Gayford M, Marston C, Cummings R, et al. Mobile clinics in humanitarian emergencies: a systematic review. Confl Health [Internet]. 2020 Dec [cited 2025 Sep 30];14(1):4. Available from: https://conflictandhealth.biomedcentral.com/articles/10.1186/s13031-020-0251-8 doi: 10.1186/s13031-020-0251-8
- Dulacha D, Ramadan OPC, Guyo AG, Maleghemi S, Wamala JF, Gimba WGW, et al. Use of mobile medical teams to fill critical gaps in health service delivery in complex humanitarian settings, 2017-2020: a case study of South Sudan. Pan Afr Med J [Internet]. 2022 Jun 9 [cited 2025 Sep 30];42 Suppl 1:8. Available from: https://www.panafrican-med-journal.com/content/series/42/1/8/full/ doi: 10.11604/pamj.supp.2022.42.1.33865
- Gao MZ, Chou YH, Chang YZ, Pai JY, Bair H, Pai S, et al. Designing mobile epidemic prevention medical stations for the COVID-19 pandemic and international medical aid. Int J Environ Res Public Health [Internet]. 2022 Aug 12 [cited 2025 Sep 30];19(16):9959. Available from: https://www.mdpi.com/1660-4601/19/16/9959 doi: 10.3390/ijerph19169959
- Kulle AC, Schumacher S, Von Bieberstein F. Mobile vaccination units substantially increase COVID-19 vaccinations: evidence from a randomized controlled trial. J Public Health (Oxf) [Internet]. 2023 Nov 20 [cited 2025 Sep 30];46(1):151-7. Available from: https://academic.oup.com/jpubhealth/article/46/1/151/7434434 doi: 10.1093/pubmed/fdad213
- Mwakilama E, Mtumbuka F, Samikwa E. Use of e-mobile technology in building risk and disaster resilience in Southern Africa – FRG and e-CRG members join hands to develop a disaster rapid response system using mathematical optimization model. INFORMS J Optim Manag [Internet]. 2021 Apr 8 [cited 2025 Sep 30];7:45-58. Available from: https://pubsonline.informs.org/do/10.1287/orms.2021.02.15/full/
- Hermansson H. Challenges to decentralization of disaster management in Turkey: the role of political-administrative context. Int J Public Adm [Internet]. 2018 May 1 [cited 2025 Sep 30];42(5):417-31. Available from: https://www.tandfonline.com/doi/full/10.1080/01900692.2018.1466898 doi: 10.1080/01900692.2018.1466898
- Iqbal K, Ahmed M. Are decentralised governments more effective in mitigating disaster risks? Bangladesh Dev Stud [Internet]. 2015 [cited 2025 Sep 30];38(3):1-24. Available from: https://www.jstor.org/stable/26538810
- World Health Organization. Framework for a public health emergency operations centre [Internet]. Geneva (Switzerland): World Health Organization; 2015 Nov 24 [cited 2025 Sep 30]. 80 p. Available from: https://www.who.int/publications/i/item/framework-for-a-public-health-emergency-operations-centre
- Fekadu ST, Gebrewahid AL, Mankoula W, Eteng W, Lokossou V, Kawe Y, et al. Public health emergency operations centres in Africa: a cross-sectional study assessing the implementation status of core components and areas for improvement, December 2021. BMJ Open [Internet]. 2023 Jun 20 [cited 2025 Sep 30];13(6):e068934. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2022-068934 doi: 10.1136/bmjopen-2022-068934
- Olu OO, Lamunu M, Chimbaru A, Adegboyega A, Conteh I, Nsenga N, et al. Incident management systems are essential for effective coordination of large disease outbreaks: perspectives from the coordination of the Ebola outbreak response in Sierra Leone. Front Public Health [Internet]. 2016 Nov 21 [cited 2025 Sep 30];4:254. Available from: http://journal.frontiersin.org/article/10.3389/fpubh.2016.00254/full doi: 10.3389/fpubh.2016.00254
- Tsukayama R, Wodniak N, Hinjoy S, Bunthi C, Akarasewi P, Jiaranairungroj W, et al. Public health emergency operations center operations and coordination among Thailand, Cambodia, Lao PDR, and Malaysia during the COVID-19 pandemic. Glob Secur [Internet]. 2023 May 29 [cited 2025 Sep 30];8(1):2216267. Available from: https://www.tandfonline.com/doi/full/10.1080/23779497.2023.2216267 doi: 10.1080/23779497.2023.2216267
- Ngoy N, Oyugi B, Ouma PO, Conteh IN, Woldetsadik SF, Nanyunja M, et al. Coordination mechanisms for COVID-19 in the WHO Regional office for Africa. BMC Health Serv Res [Internet]. 2022 May 28 [cited 2025 Sep 30];22(1):711. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-022-08035-w doi: 10.1186/s12913-022-08035-w
- Eteng WEO, Lilay A, Tekeste S, Mankoula W, Collard E, Waya C, et al. Strengthening COVID-19 pandemic response coordination through public health emergency operations centres (PHEOC) in Africa: review of a multi-faceted knowledge management and sharing approach, 2020–2021. Coffee M, editor. PLOS Glob Public Health [Internet]. 2023 Jun 22 [cited 2025 Sep 30];3(6):e0001386. Available from: https://dx.plos.org/10.1371/journal.pgph.0001386 doi: 10.1371/journal.pgph.0001386
- African Union, Africa Centres for Disease Control and Prevention, World Health Organization. Joint emergency preparedness and response (EPR) action plan 2023-27 – strengthening the health emergency preparedness and response of the African continent [Internet]. Addis Ababa (Ethiopia): African Union, Africa Centres for Disease Control and Prevention, World Health Organization; 2023 Nov 17 [cited 2025 Sep 30]. 81 p. Available from: https://www.jointemergencyactionplan.com/assets/blog/Joint%20EPR%20Detailed%20Action%20Plan%20Final%20Report.pdf
- Lampaert E, Nsio Mbeta J, Nair D, Mashako M, De Weggheleire A, Sprecher A, et al. Evaluation of centralised and decentralised models of care during the 2020 Ebola Virus Disease outbreak in Equateur Province, Democratic Republic of the Congo: a brief report. F1000Res [Internet]. 2024 Aug 28 [cited 2025 Sep 30];13:642. Available from: https://f1000research.com/articles/13-642/v2 doi: 10.12688/f1000research.150755.2
- Bell BP, Damon IK, Jernigan DB, Kenyon TA, Nichol ST, O’Connor JP, et al. Overview, control strategies, and lessons learned in the CDC response to the 2014–2016 Ebola epidemic. MMWR Suppl [Internet]. 2016 Jul 8 [cited 2025 Sep 30];65(3):4-11. Available from: http://www.cdc.gov/mmwr/volumes/65/su/su6503a2.htm doi: 10.15585/mmwr.su6503a2
- Kluge HHP, Jakab Z, Bartovic J, D’Anna V, Severoni S. Refugee and migrant health in the COVID-19 response. Lancet [Internet]. 2020 Mar 31 [cited 2025 Sep 30];395(10232):1237-9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673620307911 doi: 10.1016/S0140-6736(20)30791-1
- Dudley L, Couper I, Kannangarage NW, Naidoo S, Ribas CR, Koller TS, et al. COVID-19 preparedness and response in rural and remote areas: a scoping review. PLOS Glob Public Health [Internet]. 2023 Nov 15 [cited 2025 Sep 30];3(11):e0002602. Available from: https://dx.plos.org/10.1371/journal.pgph.0002602 doi: 10.1371/journal.pgph.0002602
- Africa Centres for Disease Control and Prevention. Outbreak report, 26 August 2024: mpox situation in Africa [Internet]. Addis Ababa (Ethiopia): Africa Centres for Disease Control and Prevention; 2024 Aug 28 [cited 2025 Sep 30]. 4 p. Available from: https://africacdc.org/download/outbreak-report-26-august-2024-mpox-situation-in-africa
- Africa Centres for Disease Control and Prevention. Mpox continental response plan 2.0 [Internet]. Addis Ababa (Ethiopia): Africa Centres for Disease Control and Prevention; 2025 Apr 14 [cited 2025 Sep 30]. 36 p. Available from: https://africacdc.org/download/mpox-continental-response-plan-2-0/?utm_source=chatgpt.com
- Africa Centres for Disease Control and Prevention. Africa CDC congratulates Democratic Republic of the Congo on launching mpox vaccination campaign [Internet]. Addis Ababa (Ethiopia): Africa Centres for Disease Control and Prevention; 2024 Sep 19 [cited 2025 Sep 30]. Available from: https://africacdc.org/news-item/africa-cdc-congratulates-democratic-republic-of-the-congo-on-launching-mpox-vaccination-campaign
- Kahondwa P. Mpox in the DRC: vaccination at the heart of the response [Internet]. Washington (DC): Gavi, the Vaccine Alliance; 2024 Nov 6 [cited 2025 Sep 30]. Available from: https://www.gavi.org/vaccineswork/mpox-drc-vaccination-heart-response
- Médecins Sans Frontières. DRC: MSF operating two Ebola treatment centres [Internet]. Dubai (UAE): Médecins Sans Frontières; 2014 Sep 9 [cited 2025 Sep 30]. Available from: https://www.msf-me.org/media-centre/news-and-stories/drc-msf-operating-two-ebola-treatment-centres?utm_source=chatgpt.com
- Médecins Sans Frontières. Inside the ‘MUST’: the mobile unit surgical trailer [Internet]. London (UK): Médecins Sans Frontières; 2017 Sep 7 [cited 2025 Sep 30]. Available from: https://msf.org.uk/article/inside-must-mobile-unit-surgical-trailer?utm_source=chatgpt.com
- Médecins Sans Frontières. South Sudan: MSF calls for improved and coordinated response to cholera outbreak in Upper Nile [Internet]. Nairobi (Kenya): Médecins Sans Frontières; 2024 Dec 6 [cited 2025 Sep 30]. Available from: https://msf.or.ke/news-and-resources/news/south-sudan-msf-calls-improved-and-coordinated-response-cholera-outbreak
